Article
Malaria
What is Malaria?
Malaria is a life-threatening parasitic disease transmitted by mosquitoes. It was once thought that the disease came from fetid marshes, hence the name mal aria (bad air). In 1880, scientists discovered the real cause of malaria: a one-cell parasite called plasmodium. Later they discovered that the parasite is transmitted from person to person through the bite of a female Anopheles mosquito, which requires blood to nurture her eggs.
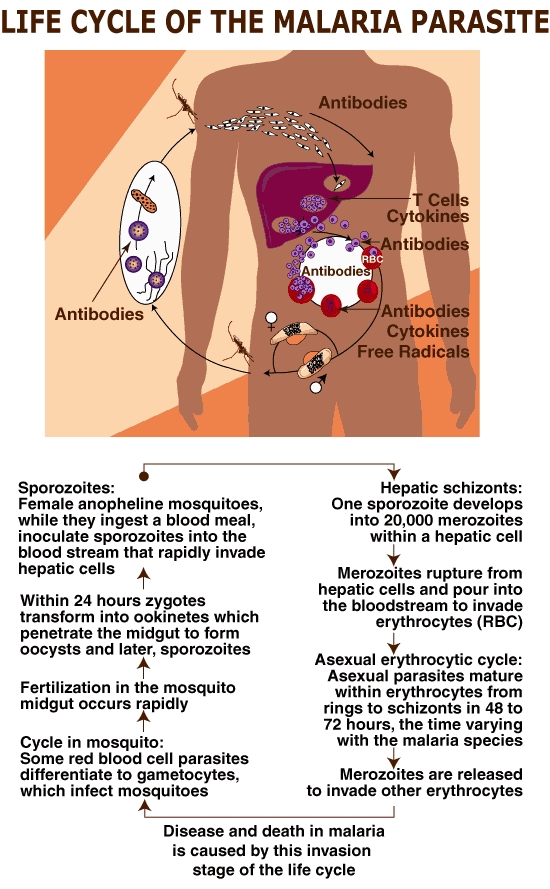
Causes and Risk Factors of Malaria
Malaria comes from being bitten by a mosquito carrying the malaria organism. Risk factors include traveling in areas in which such mosquitoes are found or, rarely, being bitten by a mosquito that has previously fed on an "imported" case of malaria (such that the case can occur in an area of the world where malaria is not endemic).Symptoms of Malaria
Malarial attacks present over 4 to 6 hours with shaking chills, high fever, and sweating, and are often associated with fatigue, headache, dizziness, nausea, vomiting, abdominal cramps, dry cough, muscle or joint pain, and back ache. The attacks may occur every other day or every third day.
Cerebral malaria and death can occur, sometimes within 24 hours, if the infection is caused by plasmodium falciparum.
Fever or other symptoms can develop in malaria as early as 8 days or as late as 60 days after exposure or stopping prophylaxis. For plasmodium vivax in temperate areas, the delay may be up to one year.Diagnosis of Malaria
Methods of diagnosis are:
- complete medical history of symptoms and travel
- physical examination
- blood tests, including thick and thin blood films, to identify the plasmodium species responsible for infectionTreatment of Malaria
Medical treatment should be sought immediately.The effectiveness of antimalarial drugs differs with different species of the parasite and with different stages of the parasite's life cycle. Your physician will determine the treatment plan most appropriate for your individual condition.
Drugs include chloroquine, mefloquine, primaquine, quinine, pyrimethamine-sulfadoxine (Fansidar), and doxycycline. Some plasmodium have developed resistance to certain medications, and therefore, alternative medications will be prescribed for you.Prevention of Malaria
No prophylactic regimen gives complete protection. Speak with your physician or local travel clinic to receive up to date information about the best malaria protection for you. Effectiveness of any given medication varies by the region of the world in which you plan to travel. Effectiveness also varies from year to year, so current information is essential.
Prevention is based on:
- evaluating the risk of exposure to infection
- preventing mosquito bites by using DEET mosquito repellant, bed nets, and clothing that covers most of the body
- chemoprophylaxis (preventive medications)Questions To Ask Your Doctor About Malaria
Are preventive measures necessary for the region of the world I'll be visiting?
Is this a high-risk area for malaria?
What drugs can be taken as a preventive measure?
What is the correct dosage?
When should the drug be started and stopped?
What other precautions should I take; repellents, clothes, nets?
What symptoms should I look for?
Swine Flu H1N1
What is Swine flu?
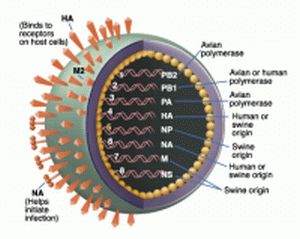
- Swine influenza, or “swine flu”, is a highly contagious acute respiratory disease of pigs, caused by one of several swine influenza A viruses.
- Swine influenza viruses are most commonly of the H1N1 subtype, but other subtypes are also circulating in pigs (e.g., H1N2, H3N1, H3N2)
- The H3N2 swine virus was thought to have been originally introduced into pigs by humans.
- Sometimes pigs can be infected with more than one virus type at a time, which can allow the genes from these viruses to mix. This can result in an influenza virus containing genes from a number of sources, called a “reassortant” virus.
- Although swine influenza viruses are normally species specific and only infect pigs, they do sometimes cross the species barrier to cause disease in humans.
- The 2009 Swine flu outbreak in humans is due to a new strain of influenza A virus subtype H1N1 that derives in part from human influenza, avian influenza, and two separate strains of swine influenza.
Modes of Transmission:
- Most infections occur among people with direct pig contact.
- Sometimes a flu virus can mutate to be more transmissible to humans.
- People who work with swine, especially people with intense exposures, are at risk of catching swine influenza if the swine carry a strain able to infect humans.
- Swine flu cannot be spread by pork products, since the virus is not transmitted through food
Signs and symptoms
The symptoms of H1N1 (swine) flu in people are similar to the symptoms of regular human flu and include fever, cough, sore throat, body aches, headache, chills and fatigue. Some people have reported diarrhea and vomiting associated with H1N1 (swine) flu. In the past, severe illness (pneumonia and respiratory failure) and deaths have been reported with H1N1 (swine) flu infection in people. Like seasonal flu, H1N1 (swine) flu may cause a worsening of underlying chronic medical conditions.
Cerebral Palsy (CP)
BASIC FACTS
Cerebral palsy (CP) is a permanent physical condition that affects movement. Its effect can be as mild as just a weakness in one hand ranging to almost complete lack of movement.
There are three main types of cerebral palsy and each involves the way a person moves. Movements can be unpredictable, muscles can be stiff or tight and in some cases people can have shaky movements or tremors.
People with cerebral palsy may have seizures and other impairments affecting their speech, vision, hearing and/or intellect.
Cerebral palsy, except in its mildest forms, can be seen in the first 12-18 months of life. It presents when children fail to reach movement milestones. Babies most at risk of cerebral palsy are those born prematurely or with low birthweight.
In Australia it is estimated that a child is born with cerebral palsy every 18 hours. Worldwide, the incidence is the same - 1 in 400 births. There is no pre-birth test and no known cure. For most, the cause is unknown.
TYPES OF CP
There are three main types of cerebral palsy:
Spastic cerebral palsy
This is the most common type of cerebral palsy. Spasticity means stiffness or tightness of muscles. The muscles are stiff because the message to the muscles is sent incorrectly through the damaged part of the brain. This is the most common type, affecting 70-80% of the people with the condition.
When people without cerebral palsy perform a movement, some groups of muscles become tighter and some groups of muscles relax. In people with spastic cerebral palsy, both groups of muscles may become tighter. This makes movement difficult or even impossible.
Dyskinetic cerebral palsy
This type affects about 10-20% of people with cerebral palsy. There are two forms:
- Athetosis is characterised by uncontrolled, slow, ‘stormy’ movements;
- Dystonia is characterised by sustained or intermittent muscle contractions causing twisting or repetitive movement.
Ataxic cerebral palsy
This is the least common type of cerebral palsy and is characterised by shaky movements. It affects a person’s balance and coordination.
Many people have signs of more than one of the three types. The most common mixed form includes spasticity and dystonic movements, but other combinations are also possible.
WHAT PART OF THE BODY IS AFFECTED BY CP?
This is different from one person to another. In cerebral palsy, certain words are used to describe the parts affected:
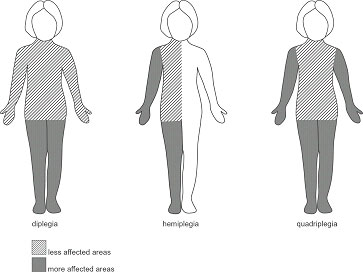
Hemiplegia - the leg and arm on one side of the body are affected.
Diplegia - both legs are affected significantly more than the arms. Children with diplegia usually have some clumsiness with their hand movements.
Quadriplegia - Both arms and legs are affected. The muscles of the trunk, face and mouth can also be affected.
WHAT CAUSES CEREBRAL PALSY?
Cerebral palsy results from damage to part of the brain. The term is used when the problem has occurred to the developing brain, usually before birth. For most people with cerebral palsy, the cause is unknown.
The risk is greater in babies born preterm and with low birthweight. Whilst the reasons for this remain unclear, cerebral palsy may occur as a result of problems associated with preterm birth or may indicate an injury has occurred during the pregnancy that has caused the baby to be born early.
In some cases, damage to the brain may occur:
- in the early months of pregnancy, for example, if the mother is exposed to certain infections such as German Measles;
- due to the baby not growing at the correct rate during the pregnancy;
- at any time if there is a lack of oxygen supplied to the baby. This is of particular concern during birth. Current research suggests that in some cases this may be due to abnormalities already present in the baby which affect the baby during the birth process;
- in the period shortly after birth, if an infant develops a severe infection such as meningitis or encephalitis, which, in rare cases, may result in brain damage;
- accidentally in the early years of life; for example, with a near drowning or car accident.
Ongoing research is vital for the management of cerebral palsy. An Australian CP Register has been set up to record the incidence and will guide future research in prevention, intervention and service provision.
WHAT OTHER CONDITIONS MAY PEOPLE WITH CEREBRAL PALSY HAVE?
Disorders of hearing - People with cerebral palsy sometimes also have hearing problems.
Disorders of eyesight - People with cerebral palsy may have squints or other visual problems.
Epilepsy - People with cerebral palsy may also have recurring seizures (fits).
Intellectual disability and learning difficulties - Children and adults with cerebral palsy vary widely in their intellectual and learning capabilities. Some will show the same intellectual capabilities as other children, in spite of their physical difficulties. Others will have some degree of intellectual disability, ranging from mild through to very significant.
Perceptual difficulties - Perception is making sense of information gained from the senses. This enables people to do things such as move around obstacles, judge size and shape of objects and understand how lines are connected to form letters. People with cerebral palsy can have problems with perception as the brain may have difficulty interpreting the messages it receives from the senses.
Speech difficulties - Because the muscles of the mouth may be affected, some people with cerebral palsy may find talking difficult. Some people may be mildly affected whilst others cannot say any words at all. People who cannot speak clearly may use a communication board or electronic communication device.
Eating and drinking difficulties - CP may affect the muscles that open and close the mouth and move the lips and the tongue. Some children have difficulty chewing and swallowing certain foods.
WHAT IS THE FUTURE FOR PEOPLE WITH CEREBRAL PALSY?
Cerebral Palsy is a life-long condition - generally the weakness, stiffness or unwanted movements remain throughout the person’s life. People with cerebral palsy live with it all their lives. It is important for children to receive support from an early age to ensure they have every opportunity to reach their full potential. There is, however, no cure for the condition.
Many people with cerebral palsy are healthy and live to old age. Those people with the more severe forms of the condition may have many health problems that result in a shortened life span. They may also experience signs of ageing at a much earlier age. For example a person with cerebral palsy may have problems with osteoporosis (brittle bones) from their early twenties. This disease would normally not be present in a non-disabled person until they were in their fifties, or older.
Parents often ask, 'Will my child lead a "normal" life?'
This varies from person to person. People with mild cerebral palsy often need no additional support to undertake the activities that most people enjoy. Others may need assistance to eat their meals, go to the toilet, or need special equipment to communicate or move around (wheelchairs and walkers).
New technology has made a huge difference. Using special accessing devices, people with cerebral palsy can now use computers like everyone else - to ‘surf’ the net, email friends, apply for jobs and work in regular employment. Computer based technology allows people with disabilities to operate everyday appliances, such as TVs, CD and DVD players and air conditioners.
Like the rest of the community, people with cerebral palsy have a wide range of skills, qualifications and experience. Some have abilities at work entry level, whilst many have tertiary qualifications such as TAFE certificates, diplomas and university degrees
Diabetes
What is diabetes?
Diabetes is a condition where the body is unable to automatically regulate blood glucose levels, resulting in too much glucose (a sugar) in the blood.
Glucose comes from foods that contain carbohydrate (starches and sugars); for example, breads and cereals, milk and dairy foods, fruits and some vegetables. Glucose travels in the blood stream to the muscles and other organs where it is used as fuel. Excess glucose is detoured to the liver where it is stored for future use. Glucose is the body’s preferred source of energy and our bodies need it to work efficiently, just like a car needs petrol to run.
The blood glucose level is regulated with the help of insulin, a hormone (or chemical messenger) made in the pancreas. >Insulin is the key that glucose needs to enter the body’s cells so that it can be used as fuel. Diabetes develops when the pancreas stops producing insulin (Type 1 diabetes or when the body does not respond properly to insulin (Type 2 diabetes). Insulin injections are necessary to treat Type 1 diabetes. Type 2 diabetes can usually be controlled in the first instance by regular exercise and diet. Tablets and eventually insulin injections may be needed as the disease progresses. The normal blood glucose level ranges between 3.5-7.8 mmol/l.
Over time, high blood glucose levels may damage blood vessels and nerves. These complications of diabetes can cause damage to eyes, nerves and kidneys and increase the risk of heart attack, stroke, impotence and foot problems. This damage can happen before an individual knows if they have diabetes if diabetes is undetected for a long time.
Studies have shown that if blood glucose and cholesterol levels, and blood pressure are kept within normal limits, the risk of damage to the body is reduced. Therefore, it is important to know if you have diabetes.
The symptoms of diabetes include:
- Thirst
- Frequent urination
- Tiredness or lack of energy
- Blurred vision
- Infections (eg. Thrush)
- Weight loss (in type 1 diabetes)
However, the symptoms of diabetes may not appear until blood glucose levels are above approximately 15mmol/l or higher. So, it is common to have diabetes without knowing about it.
In Australia, one adult in twelve has diabetes and the prevalence is increasing. Research has shown that for every person with known diabetes, there is another who has it but has not yet been diagnosed.
There are 3 main types of Diabetes:
- Type 1 (previously known as juvenile onset diabetes),
- Type 2 (previously known as mature onset diabetes) and
- Gestational Diabetes (occurring during pregnancy)
When should I be tested for diabetes?
Anyone 45 years old or older should consider getting tested for diabetes. If you are 45 or older and your BMI indicates that you are overweight .it is strongly recommended that you get tested. If you are younger than 45, are overweight, and have one or more of the risk factors, you should consider testing. Ask your doctor for a FPG or an OGTT. Your doctor will tell you if you have normal blood glucose, pre-diabetes, or diabetes. If your blood glucose is higher than normal but lower than the diabetes range (called pre-diabetes), have your blood glucose checked in 1 to 2 years.
What steps can delay or prevent type 2 diabetes?
A major research study, the Diabetes Prevention Program, confirmed that people who followed a low-fat, low-calorie diet, lost a modest amount of weight, and engaged in regular physical activity (walking briskly for 30 minutes, five times a week, for example) sharply reduced their chances of developing diabetes. These strategies worked well for both men and women and were especially effective for participants aged 60 and older.
How is diabetes managed?
If you are diagnosed with diabetes, you can manage it with meal planning, physical activity, and, if needed, medications.
Points to Remember
- Diabetes and pre-diabetes are diagnosed by checking blood glucose levels.
- Many people with pre-diabetes develop type 2 diabetes within 10 years.
- If you have pre-diabetes, you can delay or prevent type 2 diabetes with a low-fat, low-calorie diet, modest weight loss, and regular physical activity.
- If you are 45 or older, you should consider getting tested for diabetes. If you are 45 or older and overweight, it is strongly recommended that you get tested.
- If you are younger than 45, are overweight, and have one or more of the risk factors, you should consider testing.
Cerebral Palsy
CEREBRAL PALSY: BASIC FACTS
Cerebral palsy (CP) is a permanent physical condition that affects movement. Its effect can be as mild as just a weakness in one hand ranging to almost complete lack of movement.
There are three main types of cerebral palsy and each involves the way a person moves. Movements can be unpredictable, muscles can be stiff or tight and in some cases people can have shaky movements or tremors.
People with cerebral palsy may have seizures and other impairments affecting their speech, vision, hearing and/or intellect.
Cerebral palsy, except in its mildest forms, can be seen in the first 12-18 months of life. It presents when children fail to reach movement milestones. Babies most at risk of cerebral palsy are those born prematurely or with low birthweight.
In Australia it is estimated that a child is born with cerebral palsy every 18 hours. Worldwide, the incidence is the same - 1 in 400 births. There is no pre-birth test and no known cure. For most, the cause is unknown.
MORE DETAILS ABOUT CEREBRAL PALSY
TYPES OF CP
There are three main types of cerebral palsy:
Spastic cerebral palsy
This is the most common type of cerebral palsy. Spasticity means stiffness or tightness of muscles. The muscles are stiff because the message to the muscles is sent incorrectly through the damaged part of the brain. This is the most common type, affecting 70-80% of the people with the condition.
When people without cerebral palsy perform a movement, some groups of muscles become tighter and some groups of muscles relax. In people with spastic cerebral palsy, both groups of muscles may become tighter. This makes movement difficult or even impossible.
Dyskinetic cerebral palsy
This type affects about 10-20% of people with cerebral palsy. There are two forms:
- Athetosis is characterised by uncontrolled, slow, ‘stormy’ movements;
- Dystonia is characterised by sustained or intermittent muscle contractions causing twisting or repetitive movement.
Ataxic cerebral palsy
This is the least common type of cerebral palsy and is characterised by shaky movements. It affects a person’s balance and coordination.
Many people have signs of more than one of the three types. The most common mixed form includes spasticity and dystonic movements, but other combinations are also possible.
What part of the body is affected by CP?
This is different from one person to another. In cerebral palsy, certain words are used to describe the parts affected:
Hemiplegia - the leg and arm on one side of the body are affected.
Diplegia - both legs are affected significantly more than the arms. Children with diplegia usually have some clumsiness with their hand movements.
Quadriplegia - Both arms and legs are affected. The muscles of the trunk, face and mouth can also be affected.
WHAT CAUSES CEREBRAL PALSY?
Cerebral palsy results from damage to part of the brain. The term is used when the problem has occurred to the developing brain, usually before birth. For most people with cerebral palsy, the cause is unknown.
The risk is greater in babies born preterm and with low birthweight. Whilst the reasons for this remain unclear, cerebral palsy may occur as a result of problems associated with preterm birth or may indicate an injury has occurred during the pregnancy that has caused the baby to be born early.
In some cases, damage to the brain may occur:
- in the early months of pregnancy, for example, if the mother is exposed to certain infections such as German Measles;
- due to the baby not growing at the correct rate during the pregnancy;
- at any time if there is a lack of oxygen supplied to the baby. This is of particular concern during birth. Current research suggests that in some cases this may be due to abnormalities already present in the baby which affect the baby during the birth process;
- in the period shortly after birth, if an infant develops a severe infection such as meningitis or encephalitis, which, in rare cases, may result in brain damage;
- accidentally in the early years of life; for example, with a near drowning or car accident.
Ongoing research is vital for the management of cerebral palsy. An Australian CP Register has been set up to record the incidence and will guide future research in prevention, intervention and service provision.
WHAT OTHER CONDITIONS MAY PEOPLE WITH CEREBRAL PALSY HAVE?
Disorders of hearing - People with cerebral palsy sometimes also have hearing problems.
Disorders of eyesight - People with cerebral palsy may have squints or other visual problems.
Epilepsy - People with cerebral palsy may also have recurring seizures (fits).
Intellectual disability and learning difficulties - Children and adults with cerebral palsy vary widely in their intellectual and learning capabilities. Some will show the same intellectual capabilities as other children, in spite of their physical difficulties. Others will have some degree of intellectual disability, ranging from mild through to very significant.
Perceptual difficulties - Perception is making sense of information gained from the senses. This enables people to do things such as move around obstacles, judge size and shape of objects and understand how lines are connected to form letters. People with cerebral palsy can have problems with perception as the brain may have difficulty interpreting the messages it receives from the senses.
Speech difficulties - Because the muscles of the mouth may be affected, some people with cerebral palsy may find talking difficult. Some people may be mildly affected whilst others cannot say any words at all. People who cannot speak clearly may use a communication board or electronic communication device.
Eating and drinking difficulties - CP may affect the muscles that open and close the mouth and move the lips and the tongue. Some children have difficulty chewing and swallowing certain foods.
WHAT IS THE FUTURE FOR PEOPLE WITH CEREBRAL PALSY?
Cerebral Palsy is a life-long condition - generally the weakness, stiffness or unwanted movements remain throughout the person’s life. People with cerebral palsy live with it all their lives. It is important for children to receive support from an early age to ensure they have every opportunity to reach their full potential. There is, however, no cure for the condition.
Many people with cerebral palsy are healthy and live to old age. Those people with the more severe forms of the condition may have many health problems that result in a shortened life span. They may also experience signs of ageing at a much earlier age. For example a person with cerebral palsy may have problems with osteoporosis (brittle bones) from their early twenties. This disease would normally not be present in a non-disabled person until they were in their fifties, or older.
Parents often ask, 'Will my child lead a "normal" life?'
This varies from person to person. People with mild cerebral palsy often need no additional support to undertake the activities that most people enjoy. Others may need assistance to eat their meals, go to the toilet, or need special equipment to communicate or move around (wheelchairs and walkers).
New technology has made a huge difference. Using special accessing devices, people with cerebral palsy can now use computers like everyone else - to ‘surf’ the net, email friends, apply for jobs and work in regular employment. Computer based technology allows people with disabilities to operate everyday appliances, such as TVs, CD and DVD players and air conditioners.
Like the rest of the community, people with cerebral palsy have a wide range of skills, qualifications and experience. Some have abilities at work entry level, whilst many have tertiary qualifications such as TAFE certificates, diplomas and university degrees
Behcet's Disease
First Description
Hippocrates may have been the first physician to describe this disease, several centuries B.C. In the 1930's, a Turkish dermatologist, Hulusi Behcet, noted the triad of aphthous oral ulcers, genital lesions, and recurrent eye inflammation, and became the first physician to describe the disease in modern times. Another name for Behcet’s Disease is Behcet’s syndrome.
Who gets Behcet's Disease (the “typical” patient)?
Behcet’s disease is most common along the “Old Silk Route”, which spans the region from Japan and China in the Far East to the Mediterranean Sea, including countries such as Turkey and Iran. Although the disease is rare in the United States, sporadic cases do occur in patients who would not appear to be at risk because of their ethnic backgrounds (e.g., in Caucasians or African–Americans). The disease is not rare in regions along the Old Silk Route, but the disease’s epidemiology is not well understood. In Japan, Behcet’s disease ranks as a leading cause of blindness. Below is a magnetic resonance image (MRI) study of a Behcet's patient demonstrating central nervous system involvement (white matter changes in the pons).
Classic symptoms and signs of Behcet's Disease
Behcet’s disease is virtually unparalleled among the vasculitides in its ability to involve blood vessels of nearly all sizes and types, ranging from small arteries to large ones, and involving veins as well as arteries. Because of the diversity of blood vessels it affects, manifestations of Behcet’s may occur at many sites throughout the body. However, the disease has a predilection for certain organs and tissues; these are described below.
- Eye
- Mouth
- Skin
- Lungs
- Joints
- Brain
- Genitals
- Gastrointestinal Tract
Eye
- Behcet’s may cause either anterior uveitis (inflammation in the front of the eye) or posterior uveitis (inflammation in the back of the eye), and sometimes causes both at the same time.
- Anterior uveitis results in pain, blurry vision, light sensitivity, tearing, or redness of the eye.
- Posterior uveitis may be more dangerous and vision–threatening because it often causes fewer symptoms while damaging a crucial part of the eye — the retina.
Mouth
- Painful sores in the mouth called “aphthous ulcers”(pictured below). These are very similar in appearance to ulcers that frequently occur in the general population, usually as a result of minor trauma. In Behcet’s, however, the lesions are more numerous, more frequent, and often larger and more painful. Aphthous ulcers can be found on the lips, tongue, and inside of the cheek. Aphthous ulcers may occur singly or in clusters, but occur in virtually all patients with Behcet’s.
Skin
- Pustular skin lesions that resemble acne, but can occur nearly anywhere on the body. This rash is sometimes called “folliculitis”.
- Skin lesions called erythema nodosum: red, tender nodules that usually occur on the legs and ankles but also appear sometimes on the face, neck, or arms. Unlike erythema nodosum associated with other diseases (which heal without scars), the lesions of Behcet’s disease frequently ulcerate.
Lungs
- Aneurysms (outpouchings of blood vessel walls, caused by inflammation) of arteries in the lung, rupture of which may lead to massive lung hemorrhage.
Joints
- Arthritis or “arthralgias” (pain in the joints not accompanied by joint swelling).
Brain
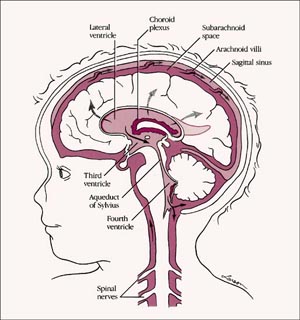
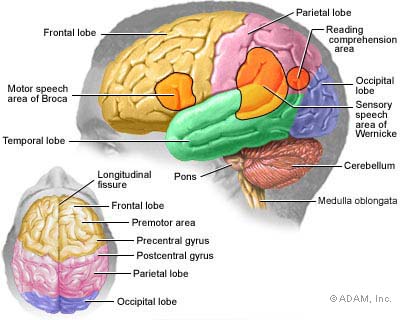
- Central nervous system involvement is one of the most dangerous manifestations of Behcet’s. The disease tends to involve the “white matter” portion of the brain and brainstem, and may lead to headaches, confusion, strokes, personality changes, and (rarely) dementia. Behcet’s may also involve the protective layers around the brain (the meninges), leading to meningitis. Because the meningitis of Behcet's disease is not associated with any known infection, it is often referred to as “aseptic” meningitis.
Genitals
- Male — painful genital lesions that form on the scrotum, similar to oral lesions, but deeper.
- Female — painful genital ulcers that develop on the vulva.
Gastrointestinal
- Ulcerations may occur anywhere in the gastrointestinal tract from the mouth to the anus. The terminal ileum and cecum are common sites. Involvement of the GI tract by Behcet’s may be difficult to distinguish from inflammatory bowel disease (such as Crohn’s disease).
What causes Behcet's Disease?
Behcet’s is one of the few forms of vasculitis in which there is a known genetic predisposition. The presence of the gene HLA–B51 is a risk factor for this disease. However, it must be emphasized that presence of the gene in and of itself is not enough to cause Behcet’s: many people possess the gene, but relatively few develop Behcet’s. Despite the predisposition to Behcet’s conferred by HLA–B51, familial cases are not the rule, constituting only about 5% of cases. Thus, it is believed that other factors (perhaps more than one) play a role. Possibilities include infections and other environmental exposures. Pictured below is a typical aphthous ulcer in a patient with Behcet's disease.
How is Behcet's Disease Diagnosed?
There is no specific “Behcet’s test”. Consequently, the diagnosis is based on the occurrence of symptoms and signs that are compatible with the disease, the presence of certain features that are particularly characteristic (e.g., oral or genital ulcerations), elimination of other possible causes of the patient’s presentation, and — whenever possible — proof of vasculitis by biopsy of an involved organ.
An international group of physicians has established a set of guidelines to aid in the classification of Behcet’s patients for the purpose of conducting research in the disease. The criteria put forth by the group include recurrent oral ulceration (at least three occasions in a year). In addition, a patient must also meet two of the following four criteria for Behcet’s disease: recurrent genital ulcerations, eye lesions (uveitis or retinal vasculitis), skin lesions (erythema nodosum, lesions, acne), and or positive "pathergy test".
The pathergy test is a simple test in which the forearm is pricked with a small, sterile needle. Occurrence of a small red bump or pustule at the site of needle insertion constitutes a positive test. Although a positive pathergy test is helpful in the diagnosis of Behcet’s, only a minority of Behcet’s patients demonstrate the pathergy phenomenon (i.e., have positive tests). Patients from the Mediterranean region are more likely to demonstrate pathergy. In addition, other conditions can occasionally result in positive pathergy tests, so the test is not 100% specific.
Pictured below is an example of the pathergy test; 1) taken at the time when the patient was “stuck” with the sterile needle; 2) shows the area immediately after the stick; 3) & 4) show the area one day and two days after the needle stick, respectively.
Treatment and Course of Behcet's Disease
For disease that is confined to mucocutaneous regions (mouth, genitals, and skin), topical steroids and non–immunosuppressive medications such as colchicine may be effective. Moderate doses of systemic corticosteroids are also frequently required for disease exacerbations, and some patients require chronic, low doses of prednisone to keep the disease under control.
In the event of serious end–organ involvement such as eye or central nervous system disease, both high doses of prednisone and some other form of immunosuppressive treatment are usually necessary. Immunosuppressive agents used in the treatment of Behcet’s include azathioprine, cyclosporine, cyclophosphamide, and chlorambucil. With organ- or life-threatening disease, the combination of prednisone and either cyclophosphamide or chlorambucil (both of which are from the same class of drug — “alkylating agents”) is the preferred therapy.
What's new in Behcet's Disease?
Thalidomide, a drug long banned in the United States because of its teratogenic potential (its ability to cause birth defects in the offspring of women who take the drug when pregnant), has been demonstrated to be effective in the treatment of mucocutaneous Behcet’s disease. Its effectiveness in more severe Behcet’s disease, however, is not known. In addition, thalidomide use is associated with the development of peripheral neuropathy (frequently irreversible) in a high percentage of patients who take the drug for prolonged periods. For more information about Thalidomide, please visit the United States Food and Drug Administration / Center for Drug Evaluation and Research’s Website on Consumer Drug Information
Interferon–alpha, a drug used in the treatment of hepatitis C, has also demonstrated some promise in Behcet’s.
Batten Disease
Introduction
Batten disease (Neuronal Ceroid Lipofuscinoses) is an inherited disorder of the nervous system that usually manifests itself in childhood.
Batten disease is named after the British paediatrician who first described it in 1903. It is one of a group of disorders called neuronal ceroid lipofuscinoses (or NCLs). Although Batten disease is the juvenile form of NCL, most doctors use the same term to describe all forms of NCL.
Early symptoms of Batten disease (or NCL) usually appear in childhood when parents or doctors may notice a child begin to develop vision problems or seizures. In some cases the early signs are subtle, taking the form of personality and behaviour changes, slow learning, clumsiness or stumbling.
Over time, affected children suffer mental impairment, worsening seizures, and progressive loss of sight and motor skills. Children become totally disabled and eventually die.
Batten disease is not contagious nor, at this time, preventable. To date it has always been fatal.
What are the forms of NCL?
There are four main types of NCL, including a very rare form that affects adults. The symptoms of all types are similar but they become apparent at different ages and progress at different rates.
- Infantile NCL: (Santavuori-Haltia type) begins between about 6 months and 2 years of age and progresses rapidly. Affected children fail to thrive and have abnormally small heads (microcephaly). Also typical are short, sharp muscle contractions called myoclonic jerks. Patients usually die before age 5, although some have survived a few years longer.
- Late infantile NCL: (Jansky-Bielschowsky type) begins between ages 2 and 4. The typical early signs are loss of muscle co-ordination (ataxia) and seizures that do not respond to anticonvulsant drugs. This form progresses fairly rapidly and children live to between the ages 6 and 12.
- Juvenile NCL: (Spielmeyer-Vogt-Sjogren Batten type) begins between the ages of 5 to 10. The most frequent beginning symptom is visual failure, less common are seizures. Motor disturbances occur late in the disease. After a slowly progressive course patients usually live to late teens, early 20’s or more rarely, into their 30’s.
- Adult NCL: (Kufs or Parry’s type) generally begins before the age of 40, causes milder symptoms that progress slowly, and does not cause blindness. Although age of death is variable among affected individuals, this form does shorten life expectancy.
- Other Types: Some children who definitely have Batten disease don't fall into any of the patterns described above. About 1 in 10 cases are not typical of any of these groups of children. In some the disease progresses more quickly and in some slower.
How many people have these disorders?
Batten disease and other forms of NCL are relatively rare, occurring in an estimated 4 of every 100,000 births in the United States. These disorders appear to be more common in Finland, Sweden, other parts of northern Europe, and Newfoundland, Canada. The incidence in Australia is not known precisely. Although NCLs are relatively rare, they can often strike more than one person in families that carry the defective gene. A family can be affected by one type of NCL only.
How are NCLs inherited?
The cause of Batten disease lies in the chromosomes, which carry the hereditary characteristics and are found in the nuclei of somatic cells. The nucleaus of every cell in the body contains twenty-three pairs of chromosomes. Each gene represents the 'code' for a particular characteristic. In the case of Batten disease, there is an aberration in one of the genes in one pair of chromosomes.
RECESSIVE MODE OF INHERITANCE
Parents
B b B b
Siblings
B B B b B b b b
Normal Carriers Affected
Childhood NCLs are autosomal recessive disorders; that is, they occur when a child inherits two copies of the defective gene, one from each parent. When this occurs, each of their children has a one in four chance of developing NCL or a one in two chance of inheriting just one copy of the defective gene. Individuals who have only one defective gene are known as carriers, meaning they do not develop the disease, but they can pass the gene onto their own children.
Although there is no conclusive test yet available to identify carriers of the affected gene, recent breakthroughs in identification of the infantile and juvenile types have brought this one step closer.
Adult NCL may be inherited as an autosomal recessive or, less often, as an autosomal dominant disorder. In autosomal dominant inheritance, all people who inherent a single copy of the disease gene develop the disease. As a result, there are no unaffected carriers of the gene.
What causes these diseases?
The defective gene causes malfunction at a cellular level. This is manifested in a number of different ways which affect the cell chemistry and leads to a variety of clinical observations and symptoms. The exact procedure in the different types of NCLs is still not understood. One theory holds that the disease reflects a disorder of the normal degradation of membranes within neurons, leading to an abnormal disposal and accumulation of insoluble lipid-protein complexes. Another theory claims that the disease may be characterised by a disorder in lipid metabolism in the cells; i.e. lipids or fats, and their associated proteins are not processed correctly.
Research suggests that there is an abnormal production of lipid peroxides and an enzyme deficiency, probably among specific enzymes that digest membrane proteins.
This combination of problems leads to the accumulation of a yellow fluorescent pigment, ceroid lipofuscin, in the brain cells. At this time, the pigment is considered to be the end result of a combination of metabolic derangements and marks the progressive deterioration in brain function.
The ceroid pigment is similar biochemically to materials accumulated more slowly during the normal ageing process. In Batten disease however, the accumulation is quite rapid and destructive. The specific reasons for the loss in brain function are not known. Thus, while there are some promising leads, and some very recent breakthroughs in gene research, we still have little understanding of the specific cause or biochemical mechanism involved in Batten disease.
Clinical course of Batten disease
Symptoms vary with each child. Early symptoms of Batten disease are confusing and not easily recognised even by medical personnel. The following is an outline of the most typical symptomatology:
- Visual impairment often progressing to complete blindness;
- Seizures, which may be frequent and difficult to control;
- Decline in cognitive function;
- Personality and behavioural changes;
- Loss of communication skills;
- Loss of fine and gross motor skills;
- Abnormal body movements;
- A general progressive deterioration.
Other symptoms that may develop include:- slowing of head growth with age in the infantile form, poor circulation in lower extremities with legs and feet cold as well as bluish-red in colour, decreased body fat and muscle mass, curvature of the spine, hyperventilation and/or breath-holding spells, difficulty in swallowing and feeding, teeth grinding and constipation.
How are these disorders diagnosed?
Batten disease is rarely diagnosed immediately because of the variability in symptoms and age of onset. Children are often mistakenly thought to have epilepsy or a form of mental retardation. Adults are sometimes labelled schizophrenics. This can be a difficult and frustrating time for all concerned.
Vision loss is often an early sign, and therefore Batten disease may be first suspected during an eye examination. A doctor can detect a loss of cells within the eye that occurs in the three childhood forms of NCL. However, because such cell loss occurs in other eye diseases, the disorder cannot be diagnosed by this sign alone. A doctor who suspects NCL may refer the child to a neurologist, a doctor who specialises in diseases of the brain and nervous system.
In order to diagnose NCL, the neurologist needs the patient’s medical history and information from various laboratory tests. Diagnostic tests used for NCLs include:
- blood or urine tests. These tests can detect abnormalities that may indicate Batten disease. For example, elevated levels of a chemical called dolichol are found in the urine of many NCL patients.
- skin or tissue sampling. The doctor can examine a small piece of tissue under a electron microscope. The powerful magnification will show typical NCL deposits. These deposits are common in skin cells, especially those from sweat glands and samples may be taken from the skin or a rectal biopsy.
- electroecephalogram or EEG. An EEG uses special patches placed on the scalp to record electrical currents inside the brain. This helps doctors see telltale patterns in the brain’s electrical activity.
- electrical studies of the eyes. These tests, which include visual-evoked responses and electroretinograms, can detect various eye problems common in childhood NCLs.
- brain scans. Imaging can help detect changes in the brain’s appearance. The most commonly used imaging technique is computed tomography, or CT, which uses x-rays and a computer to create a sophisticated picture of the brain’s tissues and structures. A second image technique that is increasingly common is magnetic resonance imaging, or MRI. MRI uses a combination of magnetic fields and radio waves, instead of radiation, to create a picture of the brain.
Tests Available
An accurate diagnosis of Batten’s disease and the particular type is essential before prenatal or presymptomatic tests can be done.
Carrier, prenatal and pre-genetic embryo (IVF) testing is available for the more common forms. Please liaise with your Medical Practitioner and a Geneticist for information.
Presymptomatic testing of younger children is possible using a skin or rectal biopsy, when the diagnosis in an older child has been confirmed with similar tests.
Is there any treatment?
As yet, no specific treatment is known that can halt or reverse the symptoms of Batten disease. However, seizures can be reduced or controlled with anti-convulsant drugs, and other medical problems can be treated appropriately as they arise. At the same time, physical and occupational therapy can help patients retain function as long as possible.
Some reports have described a slowing of the disease in children with Batten disease who were treated with vitamin supplements. Attention is being focussed on controlling some of the cell chemistry through dietary trials including fish oils and anti-oxidants. There are other studies also being carried out in the USA, UK, Australia and the Netherlands. However, so far these treatments have not prevented the final outcome of the disease.
Support and understanding can help patients and families cope with the profound disability and loss of cognitive function caused by NCLs. Often, support groups enable affected children, adults, and families to share common concerns and experiences.
Meanwhile, scientists pursue medical research that could someday (hopefully in the near future), yield an effective treatment. More government and public support are needed to provide the resources to help them.
Recent and Current Research
Through the work of several scientific teams in different countries, the search for the genetic cause of NCLs is gathering speed.
We have moved into the next decade of research since the first breakthrough of isolating the infantile gene.
Some scientists are investigating the theory that children with Batten disease have a shortage of a key body enzyme. Investigators are searching for enzymes that might be scarce, defective, or completely missing.
Trials of treatments are a reality …. Stem Cell transplants and Gene Therapy. For more information regarding these trials, please visit the BDSRA, USA via our Contacts page. Both these trials are dependent upon public funding and support.
Many animal models are available to researchers now, such as dogs (used in Australia), cow (used in Australia), sheep (used in New Zealand), fly, worm, fish and of course, mice.
Overall, while many scientists are still trying to discover the whys of Batten Disease, several others are forging ahead developing treatments
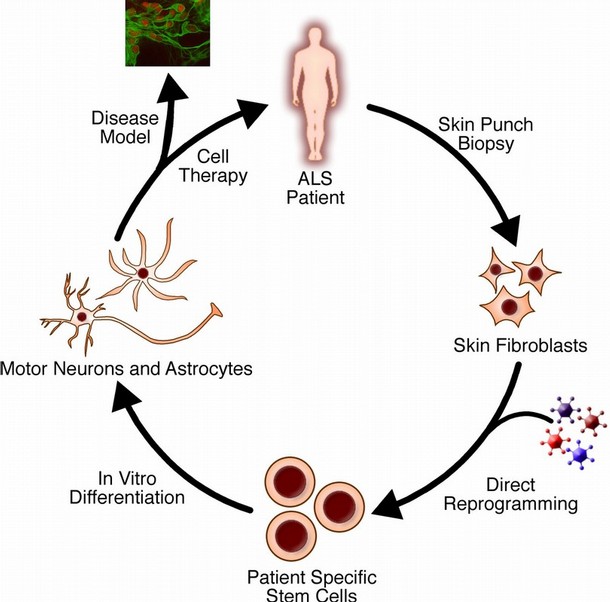
Lou Gehrig's Disease
Definition of Lou Gehrig's Disease
Lou Gehrig's Disease, also called amyotrophic lateral sclerosis (ALS), a progressive and usually fatal disorder that attacks the nerves and muscles.
It is sometimes called Lou Gehrig's disease, after the famed New York Yankee slugger whose death in 1941 was caused by this disorder.
Description of Lou Gehrig's Disease
Amyotrophic comes from the Greek language. "A" means no or negative. "Myo" refers to muscle, and "trophic" means nourishment: "No muscle nourishment."
When a muscle has no nourishment, it atrophies, or wastes away. "Lateral" identifies the areas in a person's spinal cord where portions of the nerve cells that nourish the muscles are located. As this area degenerates, it leads to scarring or "sclerosis" in the region.
ALS is a motor neuron disease. It affects the nerve cells that control the muscles we move voluntarily. In this disease, nerve cells in the brain and spinal cord, known as motor neurons, gradually degenerate, causing the muscles under their control to weaken and waste away.
ALS victims eventually become disabled, have difficulty speaking and swallowing, and may succumb to infections, particularly pneumonia.
While the disease paralyzes the "voluntary" muscles, patients remain alert and are able to think clearly, so that they can find ways to communicate without speech. The five senses are unaffected, and most patients maintain control over their bowels and bladder. For some patients, using these remaining abilities can be the springboard to cope with the disease.
The most common form of ALS is known as "sporadic" ALS. It may affect anyone at anytime.
Other terms used to categorize variants of the classical form of ALS include spinal muscular atrophy, progressive bulbar palsy and primary lateral sclerosis.
Causes and Risk Factors of Lou Gehrig's Disease
"Familial", ALS suggests the disease is inherited, although no heredity pattern exists in the majority of ALS cases. About 5 to 10 percent of all ALS patients appear to have a genetic or inherited component. In those families, 50 percent of the all offspring are expected to have the disease.
Most who develop ALS are between the ages of 40 and 70. There have been many cases of the disease attacking teenagers, though generally, ALS occurs in greater percentages as men and women grow older.
It was once believed that men developed ALS more frequently than women. That no longer appears to be the case, and today both sexes are affected in nearly equal numbers.
Symptoms of Lou Gehrig's Disease
Early symptoms vary with each individual, but they usually include tripping, dropping things, abnormal fatigue of the arms and/or legs, slurred speech, muscle cramps and twitches, and involuntary periods of laughing or crying.
With the hands and feet affected first, it causes difficulty in walking or using the hands for the activities of daily living, such as dressing, washing and buttoning clothes.
Since ALS affects only motor neurons, the senses of sight, touch, hearing, taste and smell, muscles of the eyes and bladder are generally not affected.
As the weakening and paralysis continues to spread to the muscles of the trunk of the body, it eventually affects swallowing, chewing and breathing. When the breathing muscles are affected, the patient may require permanent ventilatory support to survive. The mind is not impaired and remains sharp, despite the progressive degenerating condition of the body.
Diagnosis of Lou Gehrig's Disease
Electromyography (electrical studies of muscle) is often performed to confirm the disease. A biopsy (removal of a small piece of tissue) of muscle tissue may also been performed if the diagnosis is in doubt.
Treatment of Lou Gehrig's Disease
Although there is no cure for ALS, much can be done to help patients live more productively and independently. Physical therapy and rehabilitation techniques can help patients learn how to work around the weakness and functional disability caused by the disease. Patients may benefit from braces or a walker to improve mobility.
Questions To Ask Your Doctor About Lou Gehrig's Disease
What tests need to be done to diagnose the condition or the extent of involvement?
How fast will this progress?
What should be expected?
How long until the body begins to show signs of this condition?
Will you be prescribing any medication to relieve symptoms?
What are the side effects?
Will rehabilitative measures be started?
Is there a support group in the area?
Alzheimer's Disease
Introduction
Alzheimer’s disease is one type of dementia. It is a progressive and eventually fatal disease of the brain. It impairs higher brain functions such as memory, thinking and personality. The cause of Alzheimer’s disease is unknown and there is no cure. Current research is focusing on prevention, treatment and cure of the disease.
Two types of Alzheimer’s
The two forms of the disease are familial Alzheimer’s disease, which is caused by a rare genetic mutation, and sporadic Alzheimer’s disease, which can strike anyone. Sporadic Alzheimer’s disease affects one in 25 Australians aged 60 years and over.
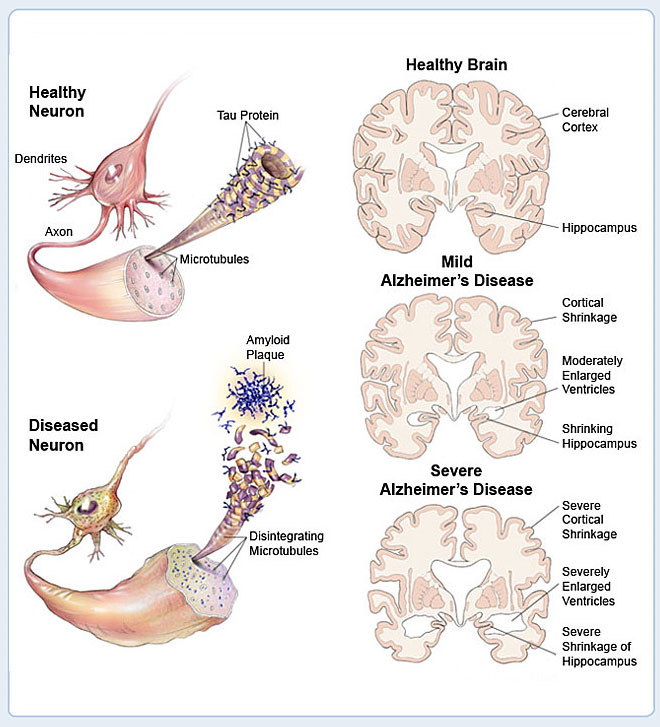
Alzheimer’s disease causes changes in the brain
How the Brain and Nerve Cells Change
|
|
|
Brain cells or neurones ‘talk’ to each other through connections called synapses. In Alzheimer’s disease, these connections are broken and ultimately disappear in the parts of the brain where thinking occurs.
Research has found that people with Alzheimer’s disease have damaged brain cells, called ‘tangles’, and deposits between the cells, called ‘amyloid plaques’. These plaques are mostly made up of a protein called ‘A-beta’ or beta amyloid. A build-up of this otherwise normal protein is thought to cause the damage.
Sometimes the beta amyloid protein can convert oxygen into hydrogen peroxide – a form of bleach – which then corrodes or ‘rusts’ brain cells, particularly the parts of the brain concerned with memory and reasoning. Researchers are trying to work out why this build-up of amyloid plaques occurs in some people and not others. They are also trying to find ways to reduce or abolish the toxic effects of this protein.
Established risk factors
The cause or causes of Alzheimer’s disease are not known. However, some risk factors have been identified. Well-established risk factors for Alzheimer’s include:
- Age – the risk of developing Alzheimer’s doubles for every five years over age 65. For people aged 70–74 years, there is a 1 in 30 chance, compared to a 1 in 3 chance for people aged 90 to 94 years.
- Genetic history – early-onset Alzheimer’s is a very rare form of the disease that can occur in people between the ages of 30 and 60. In the 1980s, researchers found that changes in certain genes cause early-onset Alzheimer’s. A person has a 1 in 2 chance of developing early-onset Alzheimer’s if one parent has any of these genetic mutations.
- Genetic conditions – most people with Down syndrome over the age of 40 will develop Alzheimer’s disease at a relatively early age. The reasons are unknown.
Possible risk factors
Other risk factors for Alzheimer’s have been suggested but not all have been proven. Some possible risk factors include:
- Head injury – especially more severe head injuries.
- Head size – people with a smaller head may be at a higher risk of Alzheimer’s disease.
- Vascular risk factors – factors that affect the vascular (blood vessel) system may also increase the risk of Alzheimer’s; these may include things such as smoking, hypertension and diabetes.
- Diet – a diet high in saturated fats may increase risk.
Research into treatments
Research into Alzheimer’s is focused on four possible treatments:
- Increase the efficiency of the damaged nerve cells – the drugs currently used are tacrine hydrochloride (Cognex) and donepezil hydrochloride (Aricept). They bolster the efficiency of the nerve cells most affected by Alzheimer’s disease. However, the effects are short lived and don’t cure the disease.
- Prevent production of beta amyloid proteins – researchers have searched for molecules which inhibit the ‘parent’ molecule of the beta amyloid protein, to reduce the production of the proteins.
- Protect nerve cells from the damaging effects of hydrogen peroxide – studies using vitamin E have shown small but significant improvements in function in one group of Alzheimer’s disease sufferers. Researchers are testing a range of antioxidants to see if they help protect nerve cells.
- Inhibit the build-up of beta amyloid proteins – researchers believe that beta amyloid proteins may become toxic as they build up. If the accumulated proteins could be broken down, they may be less harmful.
Research into risk factors and prevention
Many areas are being researched as possible risk factors, which may help identify ways to delay or prevent the onset of Alzheimer’s disease. Areas of research include:
- Cholesterol
- High blood pressure
- Diabetes
- Non-steroidal anti-inflammatory drugs (NSAIDs)
- Gender and hormones
- Brain activity
- Physical activity
- Antioxidants and nutrition.
Cholesterol
Some research has suggested a connection between high blood cholesterol levels and a higher risk of Alzheimer’s. This caused researchers to ask whether drugs that lower blood cholesterol might also lower the risk of Alzheimer’s. The most common drugs used to lower blood cholesterol are called statins. Some recent studies have shown a lower risk of dementia in people who take statins but other research has been inconclusive.
Other research has found that a high level of the amino acid homocysteine is associated with an increased risk of developing Alzheimer’s. High levels of homocysteine are known to increase heart disease risk.
High blood pressure
There may be a link between high blood pressure, other stroke risk factors and Alzheimer’s disease. High blood pressure and other stroke risk factors – age, diabetes, cardiovascular disease – can damage blood vessels in the brain and reduce the brain’s oxygen supply. This damage may disrupt nerve cell circuits that are thought to be important to decision making, memory and verbal skills.
Diabetes
Studies show that diabetes is associated with several types of dementia including Alzheimer’s and vascular dementia (a type of dementia associated with strokes). Alzheimer’s and Type 2 diabetes share several characteristics, including deposits of a damaging amyloid protein – in the brain for Alzheimer’s and in the pancreas for Type 2 diabetes. Scientists are learning more about the possible relationships between these two diseases.
Non-steroidal anti-inflammatory drugs (NSAIDs)
Non-steroidal anti-inflammatory drugs (NSAIDs) are analgesic (pain-killing) drugs used for a variety of conditions. Some studies suggest an association between a reduced risk of Alzheimer’s and the use of certain NSAIDs such as ibuprofen, naproxen and indomethacin. However, clinical trials have so far not demonstrated a benefit from these drugs.
NSAID drugs such as ibuprofen should not be taken regularly as a preventative measure against Alzheimer’s. The abuse of NSAIDs carries significant risks including stomach irritation, gastrointestinal bleeding and possible interaction with other medication.
Gender and hormones
It is known that women have a higher risk than men of developing Alzheimer’s disease, even allowing for the longer average lifespan of women. Researchers are examining the effect of various hormones on the brain, including oestrogen.
Some studies have suggested that women who take oestrogen-based hormone replacement therapy (HRT) have a lower risk of developing Alzheimer’s disease, while one recent study suggested a higher risk where oestrogen levels are low in the brain, not just in the blood. However, another study has shown that the risk of dementia does not reduce with oestrogen-only HRT, and increases slightly with combination oestrogen and progesterone therapy.
Brain activity
Keeping the brain active is associated with reduced risk of Alzheimer’s, but it is not yet clear why this is the case. Research is looking into:
- Mentally stimulating activities and how they might protect the brain. It is thought that these activities might help the brain become more adaptable and flexible in some areas of mental function so that it can compensate for declines in other areas.
- Reduced involvement in intellectual stimulation, which could reflect very early effects of the disease.
- Other lifestyle issues. People who regularly engage in mentally stimulating activities might have other lifestyle features that may protect them against Alzheimer’s.
Physical activity
Research in animals and humans has shown that both physical and mental function improve with aerobic fitness. For example, some research has found that walking was particularly beneficial. In one study, a walking group became more physically fit than those who were assigned to a stretching and toning group. The walkers also showed greater improvements on tests of planning, scheduling and decision making.
Antioxidants and nutrition
Research is continuing into the role of nutrition and nutritional supplements in Alzheimer’s disease. Areas of research include:
- Antioxidants – these may protect brain cells against the damaging effects of hydrogen peroxide as beta amyloid proteins break down. Vitamin E has shown some promise, but very high doses of vitamin E (above 1,000 units per day) can actually increase the risk of having a stroke. The herbal supplement gingko biloba is also being investigated for its antioxidant properties, but there is no evidence that it will cure or prevent Alzheimer’s.
- Fats in food – a high intake of saturated fats increases the risk of diabetes, hypertension and other vascular conditions, which are thought to be associated with Alzheimer’s. Research is investigating how diet interacts with Alzheimer’s.
- B-group vitamins – people with low levels of folic acid (folate) or vitamin B12 appear to be at higher risk of Alzheimer’s disease. A deficiency in either vitamin may allow an increase in the levels of an amino acid called homocysteine, which is known to be a risk factor for heart disease.
- Sage – the herb reputedly boosts memory. It has been shown that sage acts as a cholinesterase inhibitor, the same behaviour shown by three drugs licensed for Alzheimer’s disease.
- Aluminium – there is no evidence that aluminium in the diet or environment increases the risk of Alzheimer’s, but research is continuing.
Vitamins and herbal supplements can have powerful side effects and interact with other medication. Discuss taking any supplements with your doctor first.
Steps that may help prevent dementia and Alzheimer’s disease
It is not possible to cure dementia. There is no proven way to prevent dementia, including Alzheimer’s disease. However, research has shown that some measures may reduce the risk by either delaying or preventing the onset of dementia.
Many of these steps have proven health benefits for other conditions, even if they do not ultimately protect against Alzheimer’s disease. Suggestions include:
- Avoid head injury – always wear a seatbelt and use protective headwear for sports.
- Monitor and lower cholesterol and homocysteine levels.
- Monitor and control high blood pressure.
- Control diabetes and maintain a healthy weight.
- Limit saturated fats in your diet.
- Enjoy a diet high in antioxidants from fruits and vegetables.
- Maintain adequate dietary vitamin E and consider supplements (not more than 400mg a day) on the advice of your doctor.
- Maintain adequate B12 and folic acid intake and consider supplements on the advice of your doctor.
- Enjoy a moderate alcohol intake if you drink alcohol.
- Maintain social and intellectual activities.
- Exercise regularly.
- Don’t smoke.
Where to get help
- Your doctor
- Alzheimer’s Australia Tel. 1800 639 331
- National Dementia Helpline Tel. 1800 100 500
- The Mental Health Research Institute of Victoria Tel. (03) 9388 1633
- Your local community health service
- Your local council
- Aged Care Assessment Services (contact via DHS) Tel. (03) 9606 0000
Things to remember
- The cause of Alzheimer’s disease is not known and there is no cure.
- Research has identified many risk factors for Alzheimer’s disease.
- Activities that may prevent or delay Alzheimer’s disease will also benefit your overall health.
10 warning signs of Alzheimer's:
1. Memory loss. Forgetting recently learned information is one of the most common early signs of dementia. A person begins to forget more often and is unable to recall the information later.
What's normal? Forgetting names or appointments occasionally.
2. Difficulty performing familiar tasks. People with dementia often find it hard to plan or complete everyday tasks. Individuals may lose track of the steps involved in preparing a meal, placing a telephone call or playing a game.
What's normal? Occasionally forgetting why you came into a room or what you planned to say.
3. Problems with language. People with Alzheimer’s disease often forget simple words or substitute unusual words, making their speech or writing hard to understand. They may be unable to find the toothbrush, for example, and instead ask for "that thing for my mouth.”
What's normal? Sometimes having trouble finding the right word.
4. Disorientation to time and place. People with Alzheimer’s disease can become lost in their own neighborhood, forget where they are and how they got there, and not know how to get back home.
What's normal? Forgetting the day of the week or where you were going.
5. Poor or decreased judgment. Those with Alzheimer’s may dress inappropriately, wearing several layers on a warm day or little clothing in the cold. They may show poor judgment, like giving away large sums of money to telemarketers.
What's normal? Making a questionable or debatable decision from time to time.
6. Problems with abstract thinking. Someone with Alzheimer’s disease may have unusual difficulty performing complex mental tasks, like forgetting what numbers are for and how they should be used.
What's normal? Finding it challenging to balance a checkbook.
7. Misplacing things. A person with Alzheimer’s disease may put things in unusual places: an iron in the freezer or a wristwatch in the sugar bowl.
What's normal? Misplacing keys or a wallet temporarily.
8. Changes in mood or behavior. Someone with Alzheimer’s disease may show rapid mood swings – from calm to tears to anger – for no apparent reason.
What's normal? Occasionally feeling sad or moody.
9. Changes in personality. The personalities of people with dementia can change dramatically. They may become extremely confused, suspicious, fearful or dependent on a family member.
What's normal? People’s personalities do change somewhat with age.
10. Loss of initiative. A person with Alzheimer’s disease may become very passive, sitting in front of the TV for hours, sleeping more than usual or not wanting to do usual activities.
What's normal? Sometimes feeling weary of work or social obligations.
The difference between Alzheimer's and normal age-related memory changes
Someone with Alzheimer's disease symptoms |
Someone with normal age-related memory changes |
|
Forgets entire experiences |
Forgets part of an experience |
|
Rarely remembers later |
Often remembers later |
|
Is gradually unable to follow written/spoken directions |
Is usually able to follow written/spoken directions |
|
Is gradually unable to use notes as reminders |
Is usually able to use notes as reminders |
|
Is gradually unable to care for self |
Is usually able to care for self |
STAGES
| Stage 1: |
No impairment (normal function) |
|
|
Unimpaired individuals experience no memory problems and none are evident to a health care professional during a medical interview. |
|
Very mild cognitive decline (may be normal age-related changes or earliest signs of Alzheimer's disease) |
|
|
|
Individuals may feel as if they have memory lapses, especially in forgetting familiar words or names or the location of keys, eyeglasses or other everyday objects. But these problems are not evident during a medical examination or apparent to friends, family or co-workers. |
|
Mild cognitive decline |
|
|
|
Friends, family or co-workers begin to notice deficiencies. Problems with memory or concentration may be measurable in clinical testing or discernible during a detailed medical interview. Common difficulties include:
|
|
Moderate cognitive decline |
|
|
|
At this stage, a careful medical interview detects clear-cut deficiencies in the following areas:
|
|
Moderately severe cognitive decline |
|
|
|
Major gaps in memory and deficits in cognitive function emerge. Some assistance with day-to-day activities becomes essential. At this stage, individuals may:
|
|
Severe cognitive decline |
|
|
|
Memory difficulties continue to worsen, significant personality changes may emerge and affected individuals need extensive help with customary daily activities. At this stage, individuals may:
|
|
Very severe cognitive decline |
|
|
|
This is the final stage of the disease when individuals lose the ability to respond to their environment, the ability to speak and, ultimately, the ability to control movement.
|
AIDS/HIV
People have been warned about HIV and AIDS for over twenty years now. AIDS has already killed millions of people, millions more continue to become infected with HIV, and there's no cure – so AIDS will be around for a while yet.
AIDS is one of biggest problems facing the world today and nobody is beyond its reach. Everyone should know the basic facts about AIDS.
What is AIDS?
AIDS is a medical condition. People develop AIDS because HIV has damaged their natural defences against disease.
What is HIV?
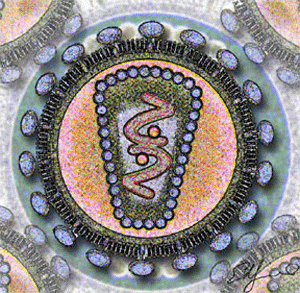
HIV (Human Immunodeficiency Virus)
HIV is a virus. Viruses infect the cells that make up the human body and replicate (make new copies of themselves) within those cells. A virus can also damage human cells, which is one of the things that can make a person ill.
HIV can be passed from one person to another. Someone can become infected with HIV through contact with the bodily fluids of someone who already has HIV.
HIV stands for the 'Human Immunodeficiency Virus'. Someone who is diagnosed as infected with HIV is said to be 'HIV+' or 'HIV positive'.
Why is HIV dangerous?
The immune system is a group of cells and organs that protect your body by fighting disease. The human immune system usually finds and kills viruses fairly quickly.
So if the body's immune system attacks and kills viruses, what's the problem?
Different viruses attack different parts of the body - some may attack the skin, others the lungs, and so on. The common cold is caused by a virus. What makes HIV so dangerous is that it attacks the immune system itself - the very thing that would normally get rid of a virus. It particularly attacks a special type of immune system cell known as a CD4 lymphocyte.
HIV has a number of tricks that help it to evade the body's defences, including very rapid mutation. This means that once HIV has taken hold, the immune system can never fully get rid of it.
There isn't any way to tell just by looking if someone's been infected by HIV. In fact a person infected with HIV may look and feel perfectly well for many years and may not know that they are infected. But as the person's immune system weakens they become increasingly vulnerable to illnesses, many of which they would previously have fought off easily.
The only reliable way to tell whether someone has HIV is for them to take a blood test, which can detect infection from a few weeks after the virus first entered the body.
When HIV causes AIDS
A damaged immune system is not only more vulnerable to HIV, but also to the attacks of other infections. It won't always have the strength to fight off things that wouldn't have bothered it before.
As time goes by, a person who has been infected with HIV is likely to become ill more and more often until, usually several years after infection, they become ill with one of a number of particularly severe illnesses. It is at this point in the stages of HIV infection that they are said to have AIDS - when they first become seriously ill, or when the number of immune system cells left in their body drops below a particular point. Different countries have slightly different ways of defining the point at which a person is said to have AIDS rather than HIV.
AIDS (Acquired Immune Deficiency Syndrome) is an extremely serious condition, and at this stage the body has very little defence against any sort of infection.
How long does HIV take to become AIDS?
Without drug treatment, HIV infection usually progresses to AIDS in an average of ten years. This average, though, is based on a person having a reasonable diet. Someone who is malnourished may well progress to AIDS and death more rapidly.
Antiretroviral medication can prolong the time between HIV infection and the onset of AIDS. Modern combination therapy is highly effective and, theoretically, someone with HIV can live for a long time before it becomes AIDS. These medicines, however, are not widely available in many poor countries around the world, and millions of people who cannot access medication continue to die.
How is HIV passed on?
HIV is found in the blood and the sexual fluids of an infected person, and in the breast milk of an infected woman. HIV transmission occurs when a sufficient quantity of these fluids get into someone else's bloodstream. There are various ways a person can become infected with HIV.
Ways in which you can be infected with HIV :
- Unprotected sexual intercourse with an infected person Sexual intercourse without a condom is risky, because the virus, which is present in an infected person's sexual fluids, can pass directly into the body of their partner. This is true for unprotected vaginal and anal sex. Oral sex carries a lower risk, but again HIV transmission can occur here if a condom is not used - for example, if one partner has bleeding gums or an open cut, however small, in their mouth.
- Contact with an infected person's blood If sufficient blood from an infected person enters someone else's body then it can pass on the virus.
- From mother to child HIV can be transmitted from an infected woman to her baby during pregnancy, delivery and breastfeeding. There are special drugs that can greatly reduce the chances of this happening, but they are unavailable in much of the developing world.
- Use of infected blood products Many people in the past have been infected with HIV by the use of blood transfusions and blood products which were contaminated with the virus - in hospitals, for example. In much of the world this is no longer a significant risk, as blood donations are routinely tested.
- Injecting drugs People who use injected drugs are also vulnerable to HIV infection. In many parts of the world, often because it is illegal to possess them, injecting equipment or works are shared. A tiny amount of blood can transmit HIV, and can be injected directly into the bloodstream with the drugs.
It is not possible to become infected with HIV through :
- sharing crockery and cutlery
- insect / animal bites
- touching, hugging or shaking hands
- eating food prepared by someone with HIV
- toilet seats
HIV facts and myths
People with HIV look just like
everybody else
Around the world, there are a number of different myths about HIV and AIDS. Here are some of the more common ones :
'You would have to drink a bucket of infected saliva to become infected yourself' . . . Yuck! This is a typical myth. HIV is found in saliva, but in quantities too small to infect someone. If you drink a bucket of saliva from an HIV positive person, you won't become infected. There has been only one recorded case of HIV transmission via kissing, out of all the many millions of kisses. In this case, both partners had extremely badly bleeding gums.
'Sex with a virgin can cure HIV' . . . This myth is common in some parts of Africa, and it is totally untrue. The myth has resulted in many rapes of young girls and children by HIV+ men, who often infect their victims. Rape won't cure anything and is a serious crime all around the world.
'It only happens to gay men / black people / young people, etc' . . . This myth is false. Most people who become infected with HIV didn't think it would happen to them, and were wrong.
'HIV can pass through latex' . . . Some people have been spreading rumours that the virus is so small that it can pass through 'holes' in latex used to make condoms. This is untrue. The fact is that latex blocks HIV, as well as sperm - preventing pregnancy, too.
What does 'safe sex' mean?
Safe sex refers to sexual activities which do not involve any blood or sexual fluid from one person getting into another person's body. If two people are having safe sex then, even if one person is infected, there is no possibility of the other person becoming infected. Examples of safe sex are cuddling, mutual masturbation, 'dry' (or 'clothed') sex . . .
In many parts of the world, particularly the USA, people are taught that the best form of safe sex is no sex - also called 'sexual abstinence'. Abstinence isn't a form of sex at all - it involves avoiding all sexual activity. Usually, young people are taught that they should abstain sexually until they marry, and then remain faithful to their partner. This is a good way for someone to avoid HIV infection, as long as their husband or wife is also completely faithful and doesn't infect them.
What is 'safer sex'?
Safer sex is used to refer to a range of sexual activities that hold little risk of HIV infection.
Safer sex is often taken to mean using a condom for sexual intercourse. Using a condom makes it very hard for the virus to pass between people when they are having sexual intercourse. A condom, when used properly, acts as a physical barrier that prevents infected fluid getting into the other person's body.
Is kissing risky?
Kissing someone on the cheek, also known as social kissing, does not pose any risk of HIV transmission.
Deep or open-mouthed kissing is considered a very low risk activity for transmission of HIV. This is because HIV is present in saliva but only in very minute quantities, insufficient to lead to HIV infection alone.
There has only been one documented instance of HIV infection as a result of kissing out of all the millions of cases recorded. This was as a result of infected blood getting into the mouth of the other person during open-mouthed kissing, and in this instance both partners had seriously bleeding gums.
Can anything 'create' HIV?
No. Unprotected sex, for example, is only risky if one partner is infected with the virus. If your partner is not carrying HIV, then no type of sex or sexual activity between you is going to cause you to become infected - you can't 'create' HIV by having unprotected anal sex, for example.
You also can't become infected through masturbation. In fact nothing you do on your own is going to give you HIV - it can only be transmitted from another person who already has the virus.
Is there a cure for AIDS?
HIV medication can slow the progress of the virus
Worryingly, surveys show that many people think that there's a 'cure' for AIDS - which makes them feel safer, and perhaps take risks that they otherwise shouldn't. These people are wrong, though - there is still no cure for AIDS.
There is antiretroviral medication which slows the progression from HIV to AIDS, and which can keep some people healthy for many years. In some cases, the antiretroviral medication seems to stop working after a number of years, but in other cases people can recover from AIDS and live with HIV for a very long time. But they have to take powerful medication every day of their lives, sometimes with very unpleasant side effects.
There is still no way to cure AIDS, and at the moment the only way to remain safe is not to become infected.
There is no cure for AIDS. Although antiretroviral treatment can suppress HIV – the virus that causes AIDS – and can delay illness for many years, it cannot clear the virus completely. There is no confirmed case of a person getting rid of HIV infection. Sadly, this doesn’t stop countless quacks and con artists touting unproven, often dangerous “AIDS cures” to desperate people.
It is easy to see why an HIV positive person might want to believe in an AIDS cure. Access to antiretroviral treatment is scarce in much of the world. When someone has a life-threatening illness they may clutch at anything to stay alive. And even when antiretroviral treatment is available, it is far from an easy solution. Drugs must be taken every day for the rest of a person’s life, often causing unpleasant side effects. A one-off cure to eradicate the virus once and for all is much more appealing.
Distrust of Western medicine is not uncommon, especially in developing countries. The Internet abounds with rumours of the pharmaceutical industry or the U.S. government suppressing AIDS cures to protect the market for patented drugs. Many people would prefer a remedy that is “natural” or “traditional”.
Where’s the harm in fake AIDS cures?
Unproven AIDS cures have been around since the syndrome emerged in the early 1980s. In most cases, they have only served to worsen suffering.
First of all, fake cures are a swindle. Someone who invests their savings in a worthless potion or an electrical zapper has less money to spend on real medicines and healthy food.
Many peddlers of bogus cures insist their clients avoid all other treatments, including antiretroviral medicines. By the time a patient realises the “cure” hasn’t worked, their prospects for successful antiretroviral treatment may well have diminished.
Fake cures may also cause direct harm to health. Inventors often refuse to reveal their recipes. Some so-called cures have been found to contain industrial solvents, disinfectants and other poisons. The dangers posed by the virgin cleansing myth – which advocates sex with children as a cure for AIDS – are only too clear.
Finally, the promotion of fake AIDS cures undermines HIV prevention. People who believe in a cure are less likely to fear becoming infected with HIV, and hence less likely to take precautions.
Why is it so difficult to cure AIDS?
Curing AIDS is generally taken to mean clearing the body of HIV, the virus that causes AIDS. The virus replicates (makes new copies of itself) by inserting its genetic code into human cells, particularly a type known as CD4 cells. Usually the infected cells produce numerous HIV particles and die soon afterwards. Antiretroviral drugs interfere with this replication process, which is why the drugs are so effective at reducing the amount of HIV in a person’s body to extremely low levels. During treatment, the concentration of HIV in the blood often falls so low that it cannot be detected by the standard test, known as a viral load test.
Unfortunately, not all infected cells behave the same way. Probably the most important problem is posed by “resting” CD4 cells. Once infected with HIV, these cells, instead of producing new copies of the virus, lie dormant for many years or even decades. Current therapies cannot remove HIV’s genetic material from these cells. Even if someone takes antiretroviral drugs for many years they will still have some HIV hiding in various parts of their body. Studies have found that if treatment is removed then HIV can re-establish itself by leaking out of these “viral reservoirs”.
A cure for AIDS must somehow remove every single one of the infected cells.
Reputable research on curing AIDS
A wide range of strategies – including such drastic measures as bone marrow transplantation – have failed in trials to eradicate HIV infection. Currently many researchers believe the best approach is to combine antiretroviral treatment with drugs that flush HIV from its hiding places. The idea is to force resting CD4 cells to become active, whereupon they will start producing new HIV particles. The activated cells should soon die or be destroyed by the immune system, and the antiretroviral medication should mop up the released HIV.
Early attempts to employ this technique used interleukin-2 (also known as IL-2 or by the brand name Proleukin). This chemical messenger tells the body to create more CD4 cells and to activate resting cells. Researchers who gave interleukin-2 together with antiretroviral treatment discovered they could no longer find any infected resting CD4 cells. But interleukin-2 failed to clear all of the HIV; as soon as the patients stopped taking antiretroviral drugs the virus came back again.1 2
There is a problem with creating a massive number of active CD4 cells: despite the antiretroviral drugs, HIV may manage to infect a few of these cells and replicate, thus keeping the infection alive. Scientists are now investigating chemicals that don’t activate all resting CD4 cells, but only the tiny minority that are infected with HIV.
One such chemical is valproic acid, a drug already used to treat epilepsy and other conditions. In 2005 a group of researchers led by David Margolis caused a sensation when they reported that valproic acid, combined with antiretroviral treatment, had greatly reduced the number of infected resting CD4 cells in four patients. They concluded that:
“This finding, though not definitive, suggests that new approaches will allow the cure of HIV in the future.”3
Sadly, it seems such optimism was premature; more recent studies suggest that valproic acid cannot eradicate HIV.4 In fact it’s quite possible that all related approaches are flawed because the virus has other hiding places besides resting CD4 cells. There is a lot about HIV that remains unknown.
Some of the world’s top research institutions are today engaged in studies to learn more about the behaviour of HIV, resting CD4 cells and other hiding places. But the truth is that this field does not receive a lot of funding. Some people think the search for a cure is not worth much investment because the task may well be impossible.
Yet there are still those who remain hopeful, including the research charity amfAR, which in 2006 awarded nearly $1.5 million to AIDS cure researchers. Activist Martin Delaney is among those calling for an end to defeatism:
“Far too many people with HIV, as well as their doctors, have accepted the notion that a cure is not likely. No one can be certain that a cure will be found. No one can predict the future. But one thing is certain: if we allow pessimism about a cure to dominate our thinking, we surely won’t get one… We must restore our belief in a cure and make it one of the central demands of our activism.”5
How to spot fake AIDS cures and treatments
As already stated, there is no proven cure for AIDS. The best advice is to steer clear of anyone claiming otherwise. For those who find themselves tempted, here are a few pointers for spotting quack therapies.
Who makes the claims?
Try to find some information about the person or people promoting the product. What are their credentials? If someone claims to be a doctor then they should say what type of doctor, and where they got their qualifications.
What claims do they make?
Look at how the product is presented. Reputable scientists and doctors don’t use sensational terms such as “miracle breakthrough”. Also watch for evidence of poor scientific understanding; for example, no expert would refer to HIV as “the HIV virus” or “the AIDS virus”.
It is very rare for a medicine to be 100% effective for all patients. It is highly implausible that a single product could cure a wide range of unrelated diseases such as cancer, asthma, AIDS and diabetes. A real scientist would be extremely wary of making such claims.
What’s in the cure?
Many inventors won’t reveal what goes into their so-called cures. Ask yourself why this might be. Could it be that their methods wouldn’t stand up to scientific scrutiny?
It is important to remember that words like “natural” and “herbal” are no guarantee of safety. After all, hemlock and ricin (derived from castor beans) are both entirely natural and extremely toxic. As the U.S. Food and Drug Administration points out,
“Any product – synthetic or natural – potent enough to work like a drug is going to be potent enough to cause side effects.”6
What evidence do they offer?
To gain the approval of medical authorities, any new treatment must undergo very extensive testing. Countless products destroy HIV in the laboratory but are ineffective or dangerous when used by people. A proper trial involves a large group of volunteers divided randomly into two sets. One half uses the test product and the other receives a placebo (a harmless pretend medicine that looks like the real thing). During the trial, neither the scientists nor the volunteers should know who is getting which treatment. Afterwards, the results for the two groups are compared to see if the test product performed better than the placebo.
Virtually all promoters of “AIDS cures” cannot provide any data from large-scale, randomised human trials. Instead they rely on anecdotes, personal testimonies, laboratory experiments or small-scale trials with no placebo comparison. This type of evidence is always unreliable.
Personal testimonies are notoriously untrustworthy. Usually there is no way of knowing whether the people in question ever existed, let alone whether they were helped by the therapy. There have been cases of people being paid to pretend they’ve been cured. And even if a handful of people really did get better after they took the treatment, this doesn’t necessarily mean that it works; the improvements may just have been a coincidence. Many negative reports may have been left out of the promotional material.
Proving that HIV has been eradicated isn’t easy. Changes in symptoms or weight gain are not sufficient, and neither is a viral load test. Even if the test can’t detect HIV in the bloodstream (perhaps because the person has been on antiretroviral therapy), this doesn’t mean the virus has been cleared from all parts of the body. Much more thorough investigation is needed.
Beware of conspiracy theorists
Many sellers of fake medicines fall back on conspiracy theories to explain why their products haven’t undergone proper testing. They say that government agencies and the medical profession seek to suppress alternative treatments to safeguard the profits of the pharmaceutical industry.
This kind of allegation is a sure sign of a charlatan. In reality, leading scientists investigate all kinds of therapies that can’t be patented. For example, the U.S. government has funded research into using generic drugs (such as valproic acid) and human hormones (such as interleukin-2) as aids to ridding the body of HIV infection.
Do some research
Any important medical breakthrough will be reported in peer-reviewed journals such as Nature, Science or The Lancet. The mainstream media will pick up the story and leading experts will express their opinions.
Simply typing the name of a supposed cure into an Internet search engine and reading some of the resulting web pages will quickly establish whether it has widespread support. It is also worth searching an online medical database such as PubMed for scientific studies and reviews.
Consult an expert
Always talk to a doctor or other health professional before trying any medical treatment. If you need more information or a second opinion, try contacting a reputable health organisation or telephone helpline. Several American states have AIDS Fraud Task Forces dedicated to combating quackery, and local Food and Drug Administration offices can provide details of any action taken against a product or its manufacturer. Similar agencies operate in most other parts of the world.
President Jammeh’s AIDS cure

President Jammeh of The Gambia, a small country in West Africa, made a dramatic announcement in January 2007:
“I can treat asthma and HIV/AIDS and the cure is a day’s treatment. Within three days the person should be tested again and I can tell you that he/she will be negative... The mandate I have is that HIV/AIDS cases can be treated on Thursdays. That is the good news and the bad news is that I cannot treat more than ten patients every Thursday.”7
Three weeks later the president’s office released the results of viral load tests conducted on the first batch of patients. According to the official statement, “the herbal medicine and therapy administered by President Jammeh have yielded results beyond all reasonable doubts, that they are effective and can cure AIDS.”8 On closer inspection, however, the findings were far from convincing.
Of the four patients with HIV-1, one had a very high viral load, one high, one moderate, and one undetectable. Of the four patients with HIV-2, one had a low viral load and three had less than the detectable level.9
The fact that half of the patients still had detectable virus in their blood shows that the president’s cure cannot be 100% effective. More importantly, as already noted, an undetectable viral load does not prove that HIV has been eradicated. Some of the patients had previously been taking antiretroviral therapy, which often renders the virus undetectable. Apparently no evaluation was done before the president’s treatment began.
The viral load tests were conducted at a university in Dakar, Senegal, using samples of the patients’ blood. It has since emerged that the scientists who ran the tests were not aware of the samples’ origin. The Senegalese experts rebutted the president’s interpretation of their findings:
“There is no baseline ... you can’t prove that someone has been cured of AIDS from just one data point. It’s dishonest of the Gambian government to use our results in this way” - Dr. Coumba Toure Kane10
“The interpretation by the Gambian authorities of the results of HIV antibody and viral load testing on blood samples sent to my laboratory is incorrect... Of those samples that were HIV-positive (66.66%), none could be described as cured.” - Professor Souleymane Mboup11
The results of a second set of viral load tests, conducted by the National Institute of Hygiene in Morocco, were released in March 2007. For the first set of patients the numbers were similar to those found in Senegal. Among 31 other patients only six had undetectable viral loads.12
Clinical data for the third and fourth batch were released in October 2007. On this occasion the State House chose to withhold the name of the country in which the samples were tested. Twenty-seven of the seventy patients were found to have undetectable viral loads. Another twenty-seven had viral load counts above half a million, which is considered to be very high. The CD4 counts for twenty-seven of the seventy patients were below 200, which means they had progressed from HIV infection to AIDS. Curious repetitions within the viral load count data cast doubt on their accuracy.13
At least two of the president’s patients are known to have died.14
These unpromising outcomes have not shaken the president’s belief in his treatment, which is endorsed by the Gambian health ministry and is administered at state hospitals. President Jammeh, who has no medical qualifications, refuses to disclose exactly what goes into his cure. All he has revealed is that it involves seven herbs, “three of which are not from Gambia.”15 The treatment involves a green paste and a grey liquid each applied to the patient’s skin, and a yellowish tea-like drink. Even more important, according to President Jammeh, is the power of prayer:
“For everything that we do 90% we have to invoke the name of almighty Allah, and then 10% is what the herbs take care of.”16
Leading AIDS experts have expressed serious concern about President Jammeh’s exploits. According to Dr. Pedro Cahn, President of the International AIDS Society:
“It is premature and unethical to label this product a cure if it has not been thoroughly tested and proven. Furthermore, to take patients off potent combination antiretroviral therapy, which has saved millions of lives since its introduction in 1996, is shocking and irresponsible.”17
A fifth batch of 150 patients began treatment in February 2008.18
Other herbal cures

Herbal mixtures comprise the most popular form of alternative AIDS therapy. Although it is possible that some of these treatments may benefit people with HIV, none is a proven cure.
- Comforter’s Healing Gift, a South African company, produces an extract of a plant called sonneblom (not sunflower). According to Freddie Isaacs, the inventor of the treatment and a co-director of the company, this product is a cure for AIDS.19 Other spokespersons have said such claims go against company policy, and the product should be described as a nutritional supplement until it has undergone proper testing. According to some reports one of South Africa’s leading attorneys, Christine Qunta, is closely connected with Comforter’s Healing Gift. South Africa’s opposition party has laid a charge against Qunta of authorising the sale of an unlicensed medicine.20
- Dr. Sebi (born Alfredo Bowman) says his “electric foods” can cure AIDS, cancer and many other illnesses. Sebi, who has offices in Honduras and the USA, has no medical qualifications and many of his views are totally at odds with basic principles of mainstream science. In Sebi’s opinion, AIDS (like all other diseases) occurs when “the mucous membrane has been compromised”.21 He says his plant extracts cure the illness by removing the mucous. Sebi was arrested in 1987 and again in 1997 for publishing false health claims and practising medicine without a licence.22 23 He has published no verifiable evidence to support his “AIDS cure”.
- IMOD was developed by scientists from Russia and Iran. When the Iranian government unveiled the drug in February 2007, many media sources, including Iran’s Fars News Agency, described IMOD as an “AIDS cure”.24 The official IMOD website makes no such claim, but does say that human trials of the drug found it increased CD4 counts in HIV positive people.25 No study reports have been published in medical journals. The research team did not respond to emails from the author of this article.
- Khomeini (or Khomein) was invented by Professor Sheik Allagholi Elahi of Iran, who set up a clinic in Uganda to sell this so-called AIDS cure for more than $1,500 per patient. The Ugandan Ministry of Health appointed a team of experts to monitor some of the few hundred people taking the treatment. After their study showed Elahi’s claims to be false, the government banned the use and distribution of Khomeini in April 2006, and Ehahi was arrested.26
- MAB Formula One and MAB Formula Two were developed by Ghanaian doctors and ethno-botanists led by Dr. Jacob Akumoah-Boateng. According to the researchers MAB Formula One kills HIV while MAB Formula Two boosts the immune system. Dr. Akumoah-Boateng says tests in the U.S. demonstrated the disappearance of HIV and HIV antibodies after the treatment was given, though none of the findings have been published in the medical literature.27
Ubhejane, a brown liquid said to be made from 89 herbs, has been taken by many hundreds of HIV positive South Africans. Its creator, Zeblon Gwala, says Ubhejane reduces viral load and increases CD4 counts in HIV positive people. He advises that it should not be taken at the same time as antiretroviral treatment.
Ubhejane has often been referred to as a “cure for AIDS” and Gwala’s employees have reportedly promoted it as such, despite having no evidence from rigorous human trials.28 29 Scientists who have tested Ubhejane in the laboratory have stressed that they haven’t demonstrated any benefits to patients.30 South Africa’s opposition party has attempted to have Gwala prosecuted for fraud.31 In 2008, the Advertising Standards Authority of South Africa demanded the withdrawal of an advertisement stating that Ubhejane boosted immunity and reduced viral load, having found these claims to be unsubstantiated.32
Chemicals
Many people mistakenly believe that what destroys HIV in the test tube must also work in the human body. This is one reason why a number of disinfectants and other chemicals have been wrongly promoted as cures for AIDS.
- Armenicum (also known as iodine-lithium-alpha-dextrin or ILalphaD) is a type of iodophor, a chemical that slowly releases iodine when mixed with water. According to Armenian scientists Armenicum, injected into the bloodstream, acts as an antiretroviral drug by blocking the replication of HIV. They claim to have evidence that the substance reduces viral load and increases CD4 counts in HIV positive people. The inventor of Armenicum, Alexander Ilyen, once said he was convinced it would lead to an AIDS cure.33 No studies of HIV positive people treated with Armenicum have been published in peer-reviewed journals. In a report on an animal experiment published in June 2007 the Armenicum research team admits that, “The systemic therapeutic application of iodophores has not yet been accepted”.34 A BBC investigation of Armenicum in 1999 found that the health of two American men got worse after they took the drug.35
- Colloidal silver is a suspension of extremely tiny silver particles in water. Many websites say this clear, colourless liquid effectively treats a wide range of bacterial and viral infections, including HIV infection. While it is true that colloidal silver kills germs in laboratory conditions, there is no reliable evidence of any benefit in people. Contrary to the claims of many retailers, colloidal silver is not harmless. Regular use can cause an irreversible bluish-grey discolouration of the skin, known as argyria.36 Consuming very large amounts of colloidal silver may lead to neurologic problems, kidney damage, stomach distress, headaches, fatigue, and skin irritation.37 There has been at least one reported case of a man falling into a coma after ingesting colloidal silver.38 In America it is illegal for retailers to make any health claims for this product.39
- Tetrasil (or Imusil) is a substance containing tetrasilver tetroxide. A patent held by Dr. Marvin S. Antelman claims that this simple chemical compound cures AIDS by “electrocuting” HIV.40 Dr. Antelman admits his approach to AIDS is “non-conventional” and he does not trust viral load tests: “Accordingly we have patients who display viral load reduction and those that do not who are nevertheless cured of AIDS”, he has said.41 Tetrasilver tetroxide is more commonly used for disinfecting swimming pools.42 After it was promoted as an AIDS cure in Zambia the government banned Tetrasil because it has no proven benefits for people living with HIV.43 In America it is illegal to promote Tetrasil for the treatment or prevention of any disease.44
- Virodene is based on the industrial solvent dimethylformamide (DMF). In the late 1990s this chemical was touted as a possible cure for AIDS. For several years senior members of the South African government, including Thabo Mbeki, vehemently supported research into Virodene as an AIDS treatment, against the advice of medical experts. South Africa’s drug regulators have long prohibited use of Virodene as it has no proven benefits. Laboratory studies have found that DMF does not destroy HIV or inhibit its replication. The only trial of its effectiveness in humans, conducted in Tanzania, found that Virodene did not reduce viral load and had only marginal effects on the immune system.45 DMF is considered a toxic substance; workers are advised to avoid skin contact with the chemical because it may cause serious liver damage.46 47 Imunoxx, which a Namibian company markets as an immune booster, is essentially identical to Virodene.
Oxygen therapy
- Hydrogen peroxide, diluted in water, is commonly used as a bleach and a disinfectant. Some alternative health practitioners advocate drinking, injecting or bathing in weak solutions of this chemical as a cure for AIDS, flu, cancer and other illnesses. There is no evidence to support these claims. Several people have died as a result of swallowing or injecting hydrogen peroxide.48 49
- Ozone is an unstable form of oxygen gas. Ozone therapy has been proposed as a treatment or cure for many illnesses, including HIV infection. One delivery method is autohemotherapy, which involves removing some of a patient’s blood, exposing it to ozone, and then putting it back into the patient. Alternatives include pumping the gas into the rectum, drinking water containing ozone bubbles (ozonized water, which contains hydrogen peroxide), or injecting the gas into the bloodstream. Studies of ozone autohemotherapy in HIV positive people have found it has no significant effect on CD4 counts and other outcomes.50 51 According to the U.S. Food and Drug Administration, “Ozone is a toxic gas with no known useful medical application in specific, adjunctive, or preventive therapy. In order for ozone to be effective as a germicide, it must be present in a concentration far greater than that which can be safely tolerated by man and animals.”52 It is illegal for retailers in America to make any health claims for ozone generators.
Electrical zappers
- Dr. Hulda Clark (who is not a licensed medical doctor) promotes a range of products said to cure AIDS including an electrical “zapper” which, by generating low voltage electricity, is supposed to kill parasites, bacteria and viruses in the body. No proper studies of the zapper have been conducted. Dr. Clark’s methods of diagnosing HIV are highly unconventional; she believes that HIV comes from intestinal worms in the presence of benzene, and that HIV can be found in snails.53 It is therefore doubtful whether the people she claims to have cured of HIV infection were ever really infected.54 Dr. Clark left America after being taken to court for practising medicine without a licence.55 She now runs a clinic in Tijuana, Mexico, where she has also run into trouble with the authorities.56
- The Bob Beck Protocol involves a set of therapies devised by the late Dr. Bob Beck (who was not a medical doctor) that are supposed to cure AIDS, cancer and all other diseases. The four components are electric currents, magnetic pulses, colloidal silver and ozonized water. There is no good evidence that electricity can cure any infection. Claims about the healing powers of Bob Beck’s devices are based entirely on test tube studies and unverifiable anecdotes.
Immune boosters
Some so-called AIDS cures are meant to stimulate the human immune system. Since HIV makes new copies of itself by infecting active immune cells, there is a real danger that such therapies will hasten the spread of the virus rather than contain it.
- Dr. Gary R. Davis got his idea for an AIDS cure from a goat that appeared in his dreams. The late Dr. Davis never prescribed his goat serum treatment (known as BB7075) to HIV positive Americans due to legal restrictions. In 1998 one young girl, Precious Thomas, was given the serum by her mother, who stole it from Davis’ office. Some websites say the girl was cured of HIV infection, based on a viral load test conducted soon afterwards.57 In a 2006 interview, however, Precious Thomas makes clear that she is still infected with HIV.58 After being denied approval in America, Dr. Davis and his associates tried to conduct goat serum trials in Ghana. Again he was stopped because “the supporting evidence for asking for registration and use of the serum was totally inadequate”.59 In late 2006, a few months before Dr. Davis’ death, the BBC exposed an attempt by a British company to test the substance on dozens of people in Swaziland, despite the lack of toxicity tests and other necessary preliminary studies.60
- The Antidote – a drug derived from a crocodile protein – has been promoted via spam email and websites with the promise that “It kills all known deadly viruses and bacteria in the body”.61 Absolutely no scientific evidence has been offered to support this claim.
- V-1 Immunitor (or V-AIM or Immureboost) is a pink pill containing antigens taken from the pooled blood of HIV positive people. A clinic in Thailand began distributing V-1 in 2001. Demand soared when the pill’s inventor, Vichai Jirathitikal, said it had eliminated HIV in two patients.62 The Thai Ministry of Public Health responded by conducting a study of those receiving V-1; the findings were not encouraging. According to a government minister, “the pill does not have any effect on the body’s immune system, white blood cell count and amount of the virus in the blood”.63 Other studies of the so-called vaccine – all carried out by employees of its manufacturer – do not provide convincing evidence of benefit. AIDS patients treated with V-1 typically survive for a matter of weeks, as opposed to the years achieved through antiretroviral treatment.64 Although the company has said that people treated with V-1 have “serodeconverted” from HIV-positive to HIV-negative,65 this claim is based on unreliable evidence and is not taken seriously by the scientific community.66 The manufacturing and sales licences for V-1 in Thailand were revoked in April 2003.67 68 Apparently undaunted, Vichai Jirathitikal and a company called Immureboost have continued to promote the product under the new name V-AIM, describing it as a therapeutic vaccine rather than a cure for AIDS.69
Faith-based cures
Religious bodies have done much to help the response to AIDS, especially by caring for the sick. Sadly a small minority of religious leaders have abused the trust placed in them by promising to cure AIDS through faith, sometimes in exchange for money or gifts. Most reports come from sub-Saharan Africa, where evangelical Americans are among those implicated.70
One of the most startling examples of recent times concerns an Ethiopian church where thousands of HIV positive people have sought a cure in showers of holy water. At one time, pilgrims were told to trust in faith alone and to refuse medication.71 Church patriarch Abune Paulos has since endorsed the use of antiretroviral treatment:
“What we are saying is taking the drugs is neither a sin nor a crime. Both the Holy Water and the medicine are gifts of God. They neither contradict nor resist each other.”72
The virgin cleansing myth
The myth that sex with a virgin can cure sexually transmitted diseases has a long history in Europe and elsewhere. Since the emergence of the AIDS epidemic, there has been much concern that this belief might encourage the rape of children, especially in Africa where HIV is widespread. A number of horrific reports in the popular press have fuelled such anxiety.
Belief in the virgin cleansing myth has been reported from Africa, Asia, Europe and the Americas. There is no doubt that it has led to abuse of not only children but also the disabled (who are often assumed to be virgins).73 Nevertheless, the scale of the myth’s impact is disputed because it is not the only motivation behind child rape.74 75 In many cases the goal is more likely to be prevention than cure: men are seeking partners who are less likely to have HIV.
Thankfully efforts are being made to dispel the virgin cleansing myth around the world. But to effectively clamp down on child rape, such campaigns must be accompanied by changes to the cultural and legal environment that enables abuse to take place.
Spontaneous cures: Andrew Stimpson
Occasionally there are reports of HIV seeming to vanish for no obvious reason. One especially sensational story broke on 13th November 2005, when two British newspapers reported that a 25-year old Scot, Andrew Stimpson, had become the first person to be cured of HIV infection.76 77
In interviews with the two papers, Stimpson said he first suspected he might have HIV in 2002, after several weeks of feeling tired and feverish. Knowing his partner had been HIV positive for a number of years, Stimpson visited the Victoria Sexual Health Clinic in London for an HIV antibody test in May. The result was negative, but he was encouraged to return for further tests, as HIV antibodies often do not appear in the blood until several weeks or even months after initial infection.
In August 2002, Stimpson returned for three more HIV antibody tests. His first, taken on the 15th, was “indeterminate” (i.e. neither definitely positive nor negative), but the following two (taken on 20th and 23rd August) both found him to be HIV antibody positive. However, a viral load test showed the amount of virus in his blood was low, so he was not prescribed antiretroviral therapy. He made a personal choice to start taking multivitamin and mineral tablets and other dietary supplements.
For fourteen months Stimpson remained surprisingly healthy, so much so that, in October 2003, his doctor offered him a repeat test for HIV antibodies. Remarkably, the test came back negative. Two more, carried out in December 2003 and March 2004, also gave negative results.
Andrew Stimpson tried to launch a legal case against the Chelsea and Westminster NHS Trust (CWT) which had tested him, assuming his results had been mixed up with those of another client. The blood samples associated with his original positive diagnosis and his subsequent negative results were retested, and the DNA from the samples compared to his. All the samples were found to belong to Stimpson, and retesting produced the same “positive then negative” antibody results. According to Stimpson:
“After the repeat tests my doctor came into the room saying, ‘You’ve cured yourself! This is unbelievable.’”78
Andrew Stimpson’s story became an overnight media sensation. But a statement from the CWT cast doubt on the cure claims:
“It is probable that there was never any evidence of Mr Stimpson having the HIV virus but rather that there was transient evidence of an antibody response to the virus present in his bloodstream when he had the initial tests... The antibody testing is exquisitely sensitive and the smallest measure can be recorded which is probably what happened in this case.”79
A spokesperson for the CWT later said they had not categorically stated that Andrew Stimpson’s case was an example of a false positive test result, but that it was one of a number of scenarios that needed to be considered.80 The media quickly accepted the “false positive” explanation, and by the end of the month the story had ceased to be of interest to them.
The only news since then dates from June 2006, when the Guardian newspaper reported that Stimpson was still working with doctors, but that because of medical confidentiality, very little more was known about the case. However, Anna Maria Geretti, a clinical virologist at the Royal Free Hospital, was willing to speculate:
“These follow-up tests are very complicated. They could take over six months. But personally, I’m sceptical that they will find a cure from this case.”81
The most likely explanation remains the occurrence of a highly unusual false positive antibody test result. This may happen if the test detects a non-HIV antibody (i.e. a similar antibody produced against a different virus) or, theoretically, because there are somehow HIV antibodies present without an actual HIV infection. Occasionally a false positive may be the result of a faulty test, though a second backup test would normally eliminate this possibility.
Although receiving three false positive results would be exceedingly unusual, some scientists believe it is more plausible than a spontaneous cure. In any case it’s extremely unlikely that, as some newspapers suggested, the multivitamins and dietary supplements that Andrew Stimpson took would have had any effect on his “seroreversion” (the process of going from HIV antibody positive to HIV antibody negative). Millions of people living with HIV take multivitamins and minerals; while such supplements may help to maintain good general health, there is no evidence that they can eliminate HIV infection.
World Impact
To understand the devastation of AIDS, you have to understand the high mortality rate of people who develop the disease. If you counted every person in the city of Chicago, which is about 3 million, you would get the idea of how many people died worldwide from AIDS in 2000. Basically, that means that each year AIDS kills the same number of people that populate the third largest city in the United States.
More then 36 million people are infected with the HIV virus worldwide, with 25.3 million of those cases in sub-Saharan Africa. Additionally, anther 5.3 million new HIV infections occurred in 2000, which represents about 16,000 new cases per day. The regions with the greatest number of people living HIV/AIDS, according to the World Health Organization, include:
- Sub-Saharan Africa - 25.3 million
- South and Southeast Asia - 5.8 million
- Latin America - 1.4 million
- North America - 920,000
- Eastern Europe/Central Asia - 700,000
In the United States, 753,907 cases had been reported to the CDC through June 2000. However, the CDC estimates that as many as 900,000 Americans are living with HIV or AIDS.
..
HIV/AIDS History
- 1926-46 - HIV possibly spreads from monkeys to humans. No one knows for sure.
- 1959 - A man dies in Congo in what many researchers say is the first proven AIDS death.
- 1981 - The Centers for Disease Control and Prevention (CDC) notices high rate of otherwise rare cancer
- 1982 - The term AIDS is used for the first time, and CDC defines it.
- 1983/84 - American and French scientists each claim discovery of the virus that will later be called HIV.
- 1985 - The FDA approves the first HIV antibody test for blood supplies.
- 1987 - AZT is the first anti-HIV drug approved by the FDA.
- 1991 - Basketball star Magic Johnson announces that he is HIV-positive.
- 1996 - FDA approves first protease inhibitors.
- 1999 - An estimated 650,000 to 900,000 Americans living with HIV/AIDS.
- 2001 - AIDS global death toll reaches nearly 22 million.