Health Articles
Behcet's Disease
First Description
Hippocrates may have been the first physician to describe this disease, several centuries B.C. In the 1930's, a Turkish dermatologist, Hulusi Behcet, noted the triad of aphthous oral ulcers, genital lesions, and recurrent eye inflammation, and became the first physician to describe the disease in modern times. Another name for Behcet’s Disease is Behcet’s syndrome.
Who gets Behcet's Disease (the “typical” patient)?
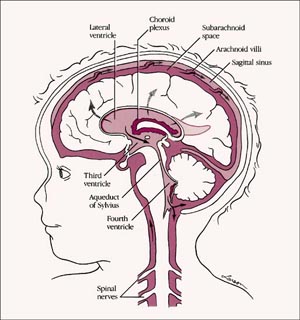
Behcet’s disease is most common along the “Old Silk Route”, which spans the region from Japan and China in the Far East to the Mediterranean Sea, including countries such as Turkey and Iran. Although the disease is rare in the United States, sporadic cases do occur in patients who would not appear to be at risk because of their ethnic backgrounds (e.g., in Caucasians or African–Americans). The disease is not rare in regions along the Old Silk Route, but the disease’s epidemiology is not well understood. In Japan, Behcet’s disease ranks as a leading cause of blindness. Below is a magnetic resonance image (MRI) study of a Behcet's patient demonstrating central nervous system involvement (white matter changes in the pons).
Classic symptoms and signs of Behcet's Disease
Behcet’s disease is virtually unparalleled among the vasculitides in its ability to involve blood vessels of nearly all sizes and types, ranging from small arteries to large ones, and involving veins as well as arteries. Because of the diversity of blood vessels it affects, manifestations of Behcet’s may occur at many sites throughout the body. However, the disease has a predilection for certain organs and tissues; these are described below.
- Eye
- Mouth
- Skin
- Lungs
- Joints
- Brain
- Genitals
- Gastrointestinal Tract
Eye
- Behcet’s may cause either anterior uveitis (inflammation in the front of the eye) or posterior uveitis (inflammation in the back of the eye), and sometimes causes both at the same time.
- Anterior uveitis results in pain, blurry vision, light sensitivity, tearing, or redness of the eye.
- Posterior uveitis may be more dangerous and vision–threatening because it often causes fewer symptoms while damaging a crucial part of the eye — the retina.
Mouth
- Painful sores in the mouth called “aphthous ulcers”(pictured below). These are very similar in appearance to ulcers that frequently occur in the general population, usually as a result of minor trauma. In Behcet’s, however, the lesions are more numerous, more frequent, and often larger and more painful. Aphthous ulcers can be found on the lips, tongue, and inside of the cheek. Aphthous ulcers may occur singly or in clusters, but occur in virtually all patients with Behcet’s.
Skin
- Pustular skin lesions that resemble acne, but can occur nearly anywhere on the body. This rash is sometimes called “folliculitis”.
- Skin lesions called erythema nodosum: red, tender nodules that usually occur on the legs and ankles but also appear sometimes on the face, neck, or arms. Unlike erythema nodosum associated with other diseases (which heal without scars), the lesions of Behcet’s disease frequently ulcerate.
Lungs
- Aneurysms (outpouchings of blood vessel walls, caused by inflammation) of arteries in the lung, rupture of which may lead to massive lung hemorrhage.
Joints
- Arthritis or “arthralgias” (pain in the joints not accompanied by joint swelling).
Brain
- Central nervous system involvement is one of the most dangerous manifestations of Behcet’s. The disease tends to involve the “white matter” portion of the brain and brainstem, and may lead to headaches, confusion, strokes, personality changes, and (rarely) dementia. Behcet’s may also involve the protective layers around the brain (the meninges), leading to meningitis. Because the meningitis of Behcet's disease is not associated with any known infection, it is often referred to as “aseptic” meningitis.
Genitals
- Male — painful genital lesions that form on the scrotum, similar to oral lesions, but deeper.
- Female — painful genital ulcers that develop on the vulva.
Gastrointestinal
- Ulcerations may occur anywhere in the gastrointestinal tract from the mouth to the anus. The terminal ileum and cecum are common sites. Involvement of the GI tract by Behcet’s may be difficult to distinguish from inflammatory bowel disease (such as Crohn’s disease).
What causes Behcet's Disease?
Behcet’s is one of the few forms of vasculitis in which there is a known genetic predisposition. The presence of the gene HLA–B51 is a risk factor for this disease. However, it must be emphasized that presence of the gene in and of itself is not enough to cause Behcet’s: many people possess the gene, but relatively few develop Behcet’s. Despite the predisposition to Behcet’s conferred by HLA–B51, familial cases are not the rule, constituting only about 5% of cases. Thus, it is believed that other factors (perhaps more than one) play a role. Possibilities include infections and other environmental exposures. Pictured below is a typical aphthous ulcer in a patient with Behcet's disease.
How is Behcet's Disease Diagnosed?
There is no specific “Behcet’s test”. Consequently, the diagnosis is based on the occurrence of symptoms and signs that are compatible with the disease, the presence of certain features that are particularly characteristic (e.g., oral or genital ulcerations), elimination of other possible causes of the patient’s presentation, and — whenever possible — proof of vasculitis by biopsy of an involved organ.
An international group of physicians has established a set of guidelines to aid in the classification of Behcet’s patients for the purpose of conducting research in the disease. The criteria put forth by the group include recurrent oral ulceration (at least three occasions in a year). In addition, a patient must also meet two of the following four criteria for Behcet’s disease: recurrent genital ulcerations, eye lesions (uveitis or retinal vasculitis), skin lesions (erythema nodosum, lesions, acne), and or positive "pathergy test".
The pathergy test is a simple test in which the forearm is pricked with a small, sterile needle. Occurrence of a small red bump or pustule at the site of needle insertion constitutes a positive test. Although a positive pathergy test is helpful in the diagnosis of Behcet’s, only a minority of Behcet’s patients demonstrate the pathergy phenomenon (i.e., have positive tests). Patients from the Mediterranean region are more likely to demonstrate pathergy. In addition, other conditions can occasionally result in positive pathergy tests, so the test is not 100% specific.
Pictured below is an example of the pathergy test; 1) taken at the time when the patient was “stuck” with the sterile needle; 2) shows the area immediately after the stick; 3) & 4) show the area one day and two days after the needle stick, respectively.
Treatment and Course of Behcet's Disease
For disease that is confined to mucocutaneous regions (mouth, genitals, and skin), topical steroids and non–immunosuppressive medications such as colchicine may be effective. Moderate doses of systemic corticosteroids are also frequently required for disease exacerbations, and some patients require chronic, low doses of prednisone to keep the disease under control.
In the event of serious end–organ involvement such as eye or central nervous system disease, both high doses of prednisone and some other form of immunosuppressive treatment are usually necessary. Immunosuppressive agents used in the treatment of Behcet’s include azathioprine, cyclosporine, cyclophosphamide, and chlorambucil. With organ- or life-threatening disease, the combination of prednisone and either cyclophosphamide or chlorambucil (both of which are from the same class of drug — “alkylating agents”) is the preferred therapy.
What's new in Behcet's Disease?
Thalidomide, a drug long banned in the United States because of its teratogenic potential (its ability to cause birth defects in the offspring of women who take the drug when pregnant), has been demonstrated to be effective in the treatment of mucocutaneous Behcet’s disease. Its effectiveness in more severe Behcet’s disease, however, is not known. In addition, thalidomide use is associated with the development of peripheral neuropathy (frequently irreversible) in a high percentage of patients who take the drug for prolonged periods. For more information about Thalidomide, please visit the United States Food and Drug Administration / Center for Drug Evaluation and Research’s Website on Consumer Drug Information
Interferon–alpha, a drug used in the treatment of hepatitis C, has also demonstrated some promise in Behcet’s.
Cerebral Palsy
CEREBRAL PALSY: BASIC FACTS
Cerebral palsy (CP) is a permanent physical condition that affects movement. Its effect can be as mild as just a weakness in one hand ranging to almost complete lack of movement.
There are three main types of cerebral palsy and each involves the way a person moves. Movements can be unpredictable, muscles can be stiff or tight and in some cases people can have shaky movements or tremors.
People with cerebral palsy may have seizures and other impairments affecting their speech, vision, hearing and/or intellect.
Cerebral palsy, except in its mildest forms, can be seen in the first 12-18 months of life. It presents when children fail to reach movement milestones. Babies most at risk of cerebral palsy are those born prematurely or with low birthweight.
In Australia it is estimated that a child is born with cerebral palsy every 18 hours. Worldwide, the incidence is the same - 1 in 400 births. There is no pre-birth test and no known cure. For most, the cause is unknown.
MORE DETAILS ABOUT CEREBRAL PALSY
TYPES OF CP
There are three main types of cerebral palsy:
Spastic cerebral palsy
This is the most common type of cerebral palsy. Spasticity means stiffness or tightness of muscles. The muscles are stiff because the message to the muscles is sent incorrectly through the damaged part of the brain. This is the most common type, affecting 70-80% of the people with the condition.
When people without cerebral palsy perform a movement, some groups of muscles become tighter and some groups of muscles relax. In people with spastic cerebral palsy, both groups of muscles may become tighter. This makes movement difficult or even impossible.
Dyskinetic cerebral palsy
This type affects about 10-20% of people with cerebral palsy. There are two forms:
- Athetosis is characterised by uncontrolled, slow, ‘stormy’ movements;
- Dystonia is characterised by sustained or intermittent muscle contractions causing twisting or repetitive movement.
Ataxic cerebral palsy
This is the least common type of cerebral palsy and is characterised by shaky movements. It affects a person’s balance and coordination.
Many people have signs of more than one of the three types. The most common mixed form includes spasticity and dystonic movements, but other combinations are also possible.
What part of the body is affected by CP?
This is different from one person to another. In cerebral palsy, certain words are used to describe the parts affected:
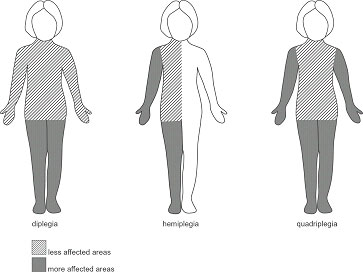
Hemiplegia - the leg and arm on one side of the body are affected.
Diplegia - both legs are affected significantly more than the arms. Children with diplegia usually have some clumsiness with their hand movements.
Quadriplegia - Both arms and legs are affected. The muscles of the trunk, face and mouth can also be affected.
WHAT CAUSES CEREBRAL PALSY?
Cerebral palsy results from damage to part of the brain. The term is used when the problem has occurred to the developing brain, usually before birth. For most people with cerebral palsy, the cause is unknown.
The risk is greater in babies born preterm and with low birthweight. Whilst the reasons for this remain unclear, cerebral palsy may occur as a result of problems associated with preterm birth or may indicate an injury has occurred during the pregnancy that has caused the baby to be born early.
In some cases, damage to the brain may occur:
- in the early months of pregnancy, for example, if the mother is exposed to certain infections such as German Measles;
- due to the baby not growing at the correct rate during the pregnancy;
- at any time if there is a lack of oxygen supplied to the baby. This is of particular concern during birth. Current research suggests that in some cases this may be due to abnormalities already present in the baby which affect the baby during the birth process;
- in the period shortly after birth, if an infant develops a severe infection such as meningitis or encephalitis, which, in rare cases, may result in brain damage;
- accidentally in the early years of life; for example, with a near drowning or car accident.
Ongoing research is vital for the management of cerebral palsy. An Australian CP Register has been set up to record the incidence and will guide future research in prevention, intervention and service provision.
WHAT OTHER CONDITIONS MAY PEOPLE WITH CEREBRAL PALSY HAVE?
Disorders of hearing - People with cerebral palsy sometimes also have hearing problems.
Disorders of eyesight - People with cerebral palsy may have squints or other visual problems.
Epilepsy - People with cerebral palsy may also have recurring seizures (fits).
Intellectual disability and learning difficulties - Children and adults with cerebral palsy vary widely in their intellectual and learning capabilities. Some will show the same intellectual capabilities as other children, in spite of their physical difficulties. Others will have some degree of intellectual disability, ranging from mild through to very significant.
Perceptual difficulties - Perception is making sense of information gained from the senses. This enables people to do things such as move around obstacles, judge size and shape of objects and understand how lines are connected to form letters. People with cerebral palsy can have problems with perception as the brain may have difficulty interpreting the messages it receives from the senses.
Speech difficulties - Because the muscles of the mouth may be affected, some people with cerebral palsy may find talking difficult. Some people may be mildly affected whilst others cannot say any words at all. People who cannot speak clearly may use a communication board or electronic communication device.
Eating and drinking difficulties - CP may affect the muscles that open and close the mouth and move the lips and the tongue. Some children have difficulty chewing and swallowing certain foods.
WHAT IS THE FUTURE FOR PEOPLE WITH CEREBRAL PALSY?
Cerebral Palsy is a life-long condition - generally the weakness, stiffness or unwanted movements remain throughout the person’s life. People with cerebral palsy live with it all their lives. It is important for children to receive support from an early age to ensure they have every opportunity to reach their full potential. There is, however, no cure for the condition.
Many people with cerebral palsy are healthy and live to old age. Those people with the more severe forms of the condition may have many health problems that result in a shortened life span. They may also experience signs of ageing at a much earlier age. For example a person with cerebral palsy may have problems with osteoporosis (brittle bones) from their early twenties. This disease would normally not be present in a non-disabled person until they were in their fifties, or older.
Parents often ask, 'Will my child lead a "normal" life?'
This varies from person to person. People with mild cerebral palsy often need no additional support to undertake the activities that most people enjoy. Others may need assistance to eat their meals, go to the toilet, or need special equipment to communicate or move around (wheelchairs and walkers).
New technology has made a huge difference. Using special accessing devices, people with cerebral palsy can now use computers like everyone else - to ‘surf’ the net, email friends, apply for jobs and work in regular employment. Computer based technology allows people with disabilities to operate everyday appliances, such as TVs, CD and DVD players and air conditioners.
Like the rest of the community, people with cerebral palsy have a wide range of skills, qualifications and experience. Some have abilities at work entry level, whilst many have tertiary qualifications such as TAFE certificates, diplomas and university degrees
Diabetes
What is diabetes?
Diabetes is a condition where the body is unable to automatically regulate blood glucose levels, resulting in too much glucose (a sugar) in the blood.
Glucose comes from foods that contain carbohydrate (starches and sugars); for example, breads and cereals, milk and dairy foods, fruits and some vegetables. Glucose travels in the blood stream to the muscles and other organs where it is used as fuel. Excess glucose is detoured to the liver where it is stored for future use. Glucose is the body’s preferred source of energy and our bodies need it to work efficiently, just like a car needs petrol to run.
The blood glucose level is regulated with the help of insulin, a hormone (or chemical messenger) made in the pancreas. >Insulin is the key that glucose needs to enter the body’s cells so that it can be used as fuel. Diabetes develops when the pancreas stops producing insulin (Type 1 diabetes or when the body does not respond properly to insulin (Type 2 diabetes). Insulin injections are necessary to treat Type 1 diabetes. Type 2 diabetes can usually be controlled in the first instance by regular exercise and diet. Tablets and eventually insulin injections may be needed as the disease progresses. The normal blood glucose level ranges between 3.5-7.8 mmol/l.
Over time, high blood glucose levels may damage blood vessels and nerves. These complications of diabetes can cause damage to eyes, nerves and kidneys and increase the risk of heart attack, stroke, impotence and foot problems. This damage can happen before an individual knows if they have diabetes if diabetes is undetected for a long time.
Studies have shown that if blood glucose and cholesterol levels, and blood pressure are kept within normal limits, the risk of damage to the body is reduced. Therefore, it is important to know if you have diabetes.
The symptoms of diabetes include:
- Thirst
- Frequent urination
- Tiredness or lack of energy
- Blurred vision
- Infections (eg. Thrush)
- Weight loss (in type 1 diabetes)
However, the symptoms of diabetes may not appear until blood glucose levels are above approximately 15mmol/l or higher. So, it is common to have diabetes without knowing about it.
In Australia, one adult in twelve has diabetes and the prevalence is increasing. Research has shown that for every person with known diabetes, there is another who has it but has not yet been diagnosed.
There are 3 main types of Diabetes:
- Type 1 (previously known as juvenile onset diabetes),
- Type 2 (previously known as mature onset diabetes) and
- Gestational Diabetes (occurring during pregnancy)
When should I be tested for diabetes?
Anyone 45 years old or older should consider getting tested for diabetes. If you are 45 or older and your BMI indicates that you are overweight .it is strongly recommended that you get tested. If you are younger than 45, are overweight, and have one or more of the risk factors, you should consider testing. Ask your doctor for a FPG or an OGTT. Your doctor will tell you if you have normal blood glucose, pre-diabetes, or diabetes. If your blood glucose is higher than normal but lower than the diabetes range (called pre-diabetes), have your blood glucose checked in 1 to 2 years.
What steps can delay or prevent type 2 diabetes?
A major research study, the Diabetes Prevention Program, confirmed that people who followed a low-fat, low-calorie diet, lost a modest amount of weight, and engaged in regular physical activity (walking briskly for 30 minutes, five times a week, for example) sharply reduced their chances of developing diabetes. These strategies worked well for both men and women and were especially effective for participants aged 60 and older.
How is diabetes managed?
If you are diagnosed with diabetes, you can manage it with meal planning, physical activity, and, if needed, medications.
Points to Remember
- Diabetes and pre-diabetes are diagnosed by checking blood glucose levels.
- Many people with pre-diabetes develop type 2 diabetes within 10 years.
- If you have pre-diabetes, you can delay or prevent type 2 diabetes with a low-fat, low-calorie diet, modest weight loss, and regular physical activity.
- If you are 45 or older, you should consider getting tested for diabetes. If you are 45 or older and overweight, it is strongly recommended that you get tested.
- If you are younger than 45, are overweight, and have one or more of the risk factors, you should consider testing.
Cerebral Palsy (CP)
BASIC FACTS
Cerebral palsy (CP) is a permanent physical condition that affects movement. Its effect can be as mild as just a weakness in one hand ranging to almost complete lack of movement.
There are three main types of cerebral palsy and each involves the way a person moves. Movements can be unpredictable, muscles can be stiff or tight and in some cases people can have shaky movements or tremors.
People with cerebral palsy may have seizures and other impairments affecting their speech, vision, hearing and/or intellect.
Cerebral palsy, except in its mildest forms, can be seen in the first 12-18 months of life. It presents when children fail to reach movement milestones. Babies most at risk of cerebral palsy are those born prematurely or with low birthweight.
In Australia it is estimated that a child is born with cerebral palsy every 18 hours. Worldwide, the incidence is the same - 1 in 400 births. There is no pre-birth test and no known cure. For most, the cause is unknown.
TYPES OF CP
There are three main types of cerebral palsy:
Spastic cerebral palsy
This is the most common type of cerebral palsy. Spasticity means stiffness or tightness of muscles. The muscles are stiff because the message to the muscles is sent incorrectly through the damaged part of the brain. This is the most common type, affecting 70-80% of the people with the condition.
When people without cerebral palsy perform a movement, some groups of muscles become tighter and some groups of muscles relax. In people with spastic cerebral palsy, both groups of muscles may become tighter. This makes movement difficult or even impossible.
Dyskinetic cerebral palsy
This type affects about 10-20% of people with cerebral palsy. There are two forms:
- Athetosis is characterised by uncontrolled, slow, ‘stormy’ movements;
- Dystonia is characterised by sustained or intermittent muscle contractions causing twisting or repetitive movement.
Ataxic cerebral palsy
This is the least common type of cerebral palsy and is characterised by shaky movements. It affects a person’s balance and coordination.
Many people have signs of more than one of the three types. The most common mixed form includes spasticity and dystonic movements, but other combinations are also possible.
WHAT PART OF THE BODY IS AFFECTED BY CP?
This is different from one person to another. In cerebral palsy, certain words are used to describe the parts affected:
Hemiplegia - the leg and arm on one side of the body are affected.
Diplegia - both legs are affected significantly more than the arms. Children with diplegia usually have some clumsiness with their hand movements.
Quadriplegia - Both arms and legs are affected. The muscles of the trunk, face and mouth can also be affected.
WHAT CAUSES CEREBRAL PALSY?
Cerebral palsy results from damage to part of the brain. The term is used when the problem has occurred to the developing brain, usually before birth. For most people with cerebral palsy, the cause is unknown.
The risk is greater in babies born preterm and with low birthweight. Whilst the reasons for this remain unclear, cerebral palsy may occur as a result of problems associated with preterm birth or may indicate an injury has occurred during the pregnancy that has caused the baby to be born early.
In some cases, damage to the brain may occur:
- in the early months of pregnancy, for example, if the mother is exposed to certain infections such as German Measles;
- due to the baby not growing at the correct rate during the pregnancy;
- at any time if there is a lack of oxygen supplied to the baby. This is of particular concern during birth. Current research suggests that in some cases this may be due to abnormalities already present in the baby which affect the baby during the birth process;
- in the period shortly after birth, if an infant develops a severe infection such as meningitis or encephalitis, which, in rare cases, may result in brain damage;
- accidentally in the early years of life; for example, with a near drowning or car accident.
Ongoing research is vital for the management of cerebral palsy. An Australian CP Register has been set up to record the incidence and will guide future research in prevention, intervention and service provision.
WHAT OTHER CONDITIONS MAY PEOPLE WITH CEREBRAL PALSY HAVE?
Disorders of hearing - People with cerebral palsy sometimes also have hearing problems.
Disorders of eyesight - People with cerebral palsy may have squints or other visual problems.
Epilepsy - People with cerebral palsy may also have recurring seizures (fits).
Intellectual disability and learning difficulties - Children and adults with cerebral palsy vary widely in their intellectual and learning capabilities. Some will show the same intellectual capabilities as other children, in spite of their physical difficulties. Others will have some degree of intellectual disability, ranging from mild through to very significant.
Perceptual difficulties - Perception is making sense of information gained from the senses. This enables people to do things such as move around obstacles, judge size and shape of objects and understand how lines are connected to form letters. People with cerebral palsy can have problems with perception as the brain may have difficulty interpreting the messages it receives from the senses.
Speech difficulties - Because the muscles of the mouth may be affected, some people with cerebral palsy may find talking difficult. Some people may be mildly affected whilst others cannot say any words at all. People who cannot speak clearly may use a communication board or electronic communication device.
Eating and drinking difficulties - CP may affect the muscles that open and close the mouth and move the lips and the tongue. Some children have difficulty chewing and swallowing certain foods.
WHAT IS THE FUTURE FOR PEOPLE WITH CEREBRAL PALSY?
Cerebral Palsy is a life-long condition - generally the weakness, stiffness or unwanted movements remain throughout the person’s life. People with cerebral palsy live with it all their lives. It is important for children to receive support from an early age to ensure they have every opportunity to reach their full potential. There is, however, no cure for the condition.
Many people with cerebral palsy are healthy and live to old age. Those people with the more severe forms of the condition may have many health problems that result in a shortened life span. They may also experience signs of ageing at a much earlier age. For example a person with cerebral palsy may have problems with osteoporosis (brittle bones) from their early twenties. This disease would normally not be present in a non-disabled person until they were in their fifties, or older.
Parents often ask, 'Will my child lead a "normal" life?'
This varies from person to person. People with mild cerebral palsy often need no additional support to undertake the activities that most people enjoy. Others may need assistance to eat their meals, go to the toilet, or need special equipment to communicate or move around (wheelchairs and walkers).
New technology has made a huge difference. Using special accessing devices, people with cerebral palsy can now use computers like everyone else - to ‘surf’ the net, email friends, apply for jobs and work in regular employment. Computer based technology allows people with disabilities to operate everyday appliances, such as TVs, CD and DVD players and air conditioners.
Like the rest of the community, people with cerebral palsy have a wide range of skills, qualifications and experience. Some have abilities at work entry level, whilst many have tertiary qualifications such as TAFE certificates, diplomas and university degrees
Swine Flu H1N1
What is Swine flu?
- Swine influenza, or “swine flu”, is a highly contagious acute respiratory disease of pigs, caused by one of several swine influenza A viruses.
- Swine influenza viruses are most commonly of the H1N1 subtype, but other subtypes are also circulating in pigs (e.g., H1N2, H3N1, H3N2)
- The H3N2 swine virus was thought to have been originally introduced into pigs by humans.
- Sometimes pigs can be infected with more than one virus type at a time, which can allow the genes from these viruses to mix. This can result in an influenza virus containing genes from a number of sources, called a “reassortant” virus.
- Although swine influenza viruses are normally species specific and only infect pigs, they do sometimes cross the species barrier to cause disease in humans.
- The 2009 Swine flu outbreak in humans is due to a new strain of influenza A virus subtype H1N1 that derives in part from human influenza, avian influenza, and two separate strains of swine influenza.
Modes of Transmission:

- Most infections occur among people with direct pig contact.
- Sometimes a flu virus can mutate to be more transmissible to humans.
- People who work with swine, especially people with intense exposures, are at risk of catching swine influenza if the swine carry a strain able to infect humans.
- Swine flu cannot be spread by pork products, since the virus is not transmitted through food
Signs and symptoms
The symptoms of H1N1 (swine) flu in people are similar to the symptoms of regular human flu and include fever, cough, sore throat, body aches, headache, chills and fatigue. Some people have reported diarrhea and vomiting associated with H1N1 (swine) flu. In the past, severe illness (pneumonia and respiratory failure) and deaths have been reported with H1N1 (swine) flu infection in people. Like seasonal flu, H1N1 (swine) flu may cause a worsening of underlying chronic medical conditions.

- Fever
- Lethargy
- Lack of appetite
- Runny nose
- Sore throat
- Coughing
- Nausea
- Vomiting
- Diarrhea
Signs and symptoms
- chills
- fever
- sore throat
- muscle pains
- severe headache
- coughing
- weakness
- general discomfort
In children emergency warning signs that need urgent medical attention include:
- Fast breathing or trouble breathing
- Bluish or gray skin color
- Not drinking enough fluids
- Severe or persistent vomiting
- Not waking up or not interacting
- Being so irritable that the child does not want to be held
- Flu-like symptoms improve but then return with fever and worse cough
In adults, emergency warning signs that need urgent medical attention include:
- Difficulty breathing or shortness of breath
- Pain or pressure in the chest or abdomen
- Sudden dizziness
- Confusion
- Severe or persistent vomiting
- Flu-like symptoms improve but then return with fever and worse cough
How does this new H1N1 virus spread?

Spread of this H1N1 virus is thought to be happening in the same way that seasonal flu spreads. Flu viruses are spread mainly from person to person through coughing or sneezing by people with influenza. Sometimes people may become infected by touching something with flu viruses on it and then touching their mouth or nose.
How long can an infected person spread this virus to others?
At the current time, CDC believes that this virus has the same properties in terms of spread as seasonal flu viruses. With seasonal flu, studies have shown that people may be contagious from one day before they develop symptoms to up to 7 days after they get sick. Children, especially younger children, might potentially be contagious for longer periods. CDC is studying the virus and its capabilities to try to learn more and will provide more information as it becomes available.
Prevention & Treatment
What can I do to protect myself from getting sick?
There is no vaccine available right now to protect against this new H1N1 virus. There are everyday actions that can help prevent the spread of germs that cause respiratory illnesses like influenza.
Take these everyday steps to protect your health:
- Cover your nose and mouth with a tissue when you cough or sneeze. Throw the tissue in the trash after you use it.
- Wash your hands often with soap and water, especially after you cough or sneeze. Alcohol-based hand cleaners are also effective.
- Avoid touching your eyes, nose or mouth. Germs spread this way.
- Try to avoid close contact with sick people.
- Stay home if you are sick for 7 days after your symptoms begin or until you have been symptom-free for 24 hours, whichever is longer. This is to keep from infecting others and spreading the virus further.
Other important actions that you can take are:
- Follow public health advice regarding school closures, avoiding crowds and other social distancing measures.
- Be prepared in case you get sick and need to stay home for a week or so; a supply of over-the-counter medicines, alcohol-based hand rubs, tissues and other related items might could be useful and help avoid the need to make trips out in public while you are sick and contagious.
Malaria
What is Malaria?
Malaria is a life-threatening parasitic disease transmitted by mosquitoes. It was once thought that the disease came from fetid marshes, hence the name mal aria (bad air). In 1880, scientists discovered the real cause of malaria: a one-cell parasite called plasmodium. Later they discovered that the parasite is transmitted from person to person through the bite of a female Anopheles mosquito, which requires blood to nurture her eggs.
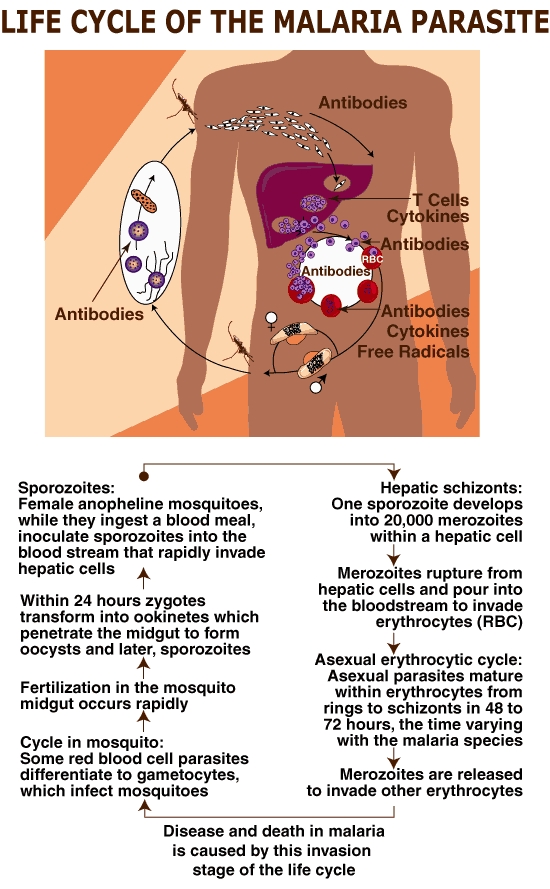
Causes and Risk Factors of Malaria
Malaria comes from being bitten by a mosquito carrying the malaria organism. Risk factors include traveling in areas in which such mosquitoes are found or, rarely, being bitten by a mosquito that has previously fed on an "imported" case of malaria (such that the case can occur in an area of the world where malaria is not endemic).Symptoms of Malaria
Malarial attacks present over 4 to 6 hours with shaking chills, high fever, and sweating, and are often associated with fatigue, headache, dizziness, nausea, vomiting, abdominal cramps, dry cough, muscle or joint pain, and back ache. The attacks may occur every other day or every third day.
Cerebral malaria and death can occur, sometimes within 24 hours, if the infection is caused by plasmodium falciparum.
Fever or other symptoms can develop in malaria as early as 8 days or as late as 60 days after exposure or stopping prophylaxis. For plasmodium vivax in temperate areas, the delay may be up to one year.Diagnosis of Malaria
Methods of diagnosis are:
- complete medical history of symptoms and travel
- physical examination
- blood tests, including thick and thin blood films, to identify the plasmodium species responsible for infectionTreatment of Malaria
Medical treatment should be sought immediately.The effectiveness of antimalarial drugs differs with different species of the parasite and with different stages of the parasite's life cycle. Your physician will determine the treatment plan most appropriate for your individual condition.
Drugs include chloroquine, mefloquine, primaquine, quinine, pyrimethamine-sulfadoxine (Fansidar), and doxycycline. Some plasmodium have developed resistance to certain medications, and therefore, alternative medications will be prescribed for you.Prevention of Malaria
No prophylactic regimen gives complete protection. Speak with your physician or local travel clinic to receive up to date information about the best malaria protection for you. Effectiveness of any given medication varies by the region of the world in which you plan to travel. Effectiveness also varies from year to year, so current information is essential.
Prevention is based on:
- evaluating the risk of exposure to infection
- preventing mosquito bites by using DEET mosquito repellant, bed nets, and clothing that covers most of the body
- chemoprophylaxis (preventive medications)Questions To Ask Your Doctor About Malaria
Are preventive measures necessary for the region of the world I'll be visiting?
Is this a high-risk area for malaria?
What drugs can be taken as a preventive measure?
What is the correct dosage?
When should the drug be started and stopped?
What other precautions should I take; repellents, clothes, nets?
What symptoms should I look for?
Ayurveda and its Origin
What is Ayurveda ?
It may be little known and remarkably few people seem to have heard of it – but ayurveda is a highly respected, highly revered ancient form of learning which has an amazing amount to teach us. It brings peace of body and mind, important ways of seeing the world and your own place in the scheme of things, and highly practical, sensible ideas when it comes to medicine, dietand ways of staying calm and relaxed
The Orgins of Ayurveda
The Origins of Ayurveda are uncertain. It is recounted that thousands of years ago, men of wisdom or rishis (meaning seers) as they are known in India, were saddened by the suffering of humanityThey knew that ill health and short lives allowed man little time to consider his spirituality and to commune with the divine - with God.
In the Himalayan mountains they prayed hard and meditated together; calling upon God to help them to relieve the plight of man, and God felt moved by compassion and gave them the essential teachings that would enlighten them in the ways of healing illness,
and thereby alleviate and remove all suffering on the earth.
It is believed that these teachings are the Vedas, although this cannot be proven, due to the lack of historical records. A book called the Atharva Veda was one of the first detailed accounts of the system. From this, and perhaps other ancient writings, came
The beginnings of Ayurvedic medicine which has developed changed and absorbed many other influences over hundreds of years to become what it is today. Due to the invasions of India over the years and the subsequent suppression if many original Indian ways of life, several ancient texts have been lost or even destroyed, but enough have survived to ensure the active continuation of these highly valued greatly respected teachings.
Ayurveda is now acknowledged as the traditional healing system of India. It comes from two Sanskrit words, ayur, Meaning “life” and veda meaning “knowing” and can be interpreted as meaning the “Science of Life”. The oldest healing system to remain intact, it is very comprehensive and has influenced many healing systems around the world
For more details about Ayurvedic Body Types
Click here :
http://www.byhealth.com/body-types
Body Types
In Ayurveda, people are classified according to three principles
Find what type of body type you are!!!
|
|
Vata |
Pitta |
Kapha |
|
Height |
Very short, tall or thin |
Medium |
Tall or short or sturdy |
|
Musculature |
Thin, Prominent tendons |
Medium/firm |
Plentiful/solid |
|
Bodily Frame |
Light narrow |
Medium frame |
Large/broad |
|
Weight |
Light, hard to gain |
Medium weight |
Heavy gains easily |
|
Sweat |
Minimal |
Profuse, especially when hot |
Moderate |
|
Skin |
Dry, Cold |
Soft, warm |
Moist, cool, possibly oily |
|
Complexion |
Darkish |
Fair, Pink, red, Fine |
Pale, white |
|
Hair Amount |
Average amount |
Early thinning and greying |
plentiful |
|
Type of Hair |
Dry, Thin, dark, Coarse |
Fine, soft red, fair |
Thick, lustrous, brown |
|
Size of Eyes |
Small, narrow or sunken |
Average |
Large, prominent |
|
Type of Eyes |
Dark brown or grey or dull |
Blue/grey/hazel, intense |
Blue, brown, attractive |
|
Teeth and Gums |
Protruding, receding gums |
Yellowish, Gums bleed |
White teeth, strong gums |
|
Size of Teeth |
Small or Large, irregular |
Average |
Large |
|
Physical Activity |
Moves quickly, active |
Moderate pace, average |
Slow, pace, steady |
|
Endurance |
Low |
good |
Very good |
|
Strength |
Poor |
good |
Very good |
|
Temperature |
Dislikes cold, likes warmth |
Likes coolness |
Aversion to cool and damp |
|
Stools |
Tendency to constipation |
Tendency to loose stools |
Plentiful, slow elimination |
|
Lifestyle |
Variable, erratic |
Busy tends to achieve a lot |
Steady can skip meals |
|
Sleep |
Light, interrupted, fitful |
Sound, Short |
Deep, likes plenty |
|
Emotional Tendency |
Fearful, anxious, insecure |
Fiery, angry, judgemental |
Greedy, Possesive |
|
Mental Activity |
Restless lots of ideas |
Sharp, precise, logical |
Calm,Steady,Stable |
|
Memory |
Good recent memory |
Sharp, Generally good |
Good long term |
|
Reaction to Stress |
Excites very easily |
Quick Temper |
Not easily irritated |
|
Work |
Creative |
intellectual |
Caring |
|
Moods |
Change Quickly |
Change Slowly |
Generally steady |
|
Speech |
Fast |
Clear, sharp, precise |
Deep, slow |
|
Resting Pulse |
|
|
|
|
Above 80 |
70-80 |
Below 70 |
|
Above 70 |
60-70 |
Below 60 |
Vata
Vata types are known to be rather restless, cool people, who certainly notice the cold, When you have excess levels of vata, fear, depression and nervousness become quite marked significant traits, and with repressed emotions comes a definite weakening of the immune system. However by adapting the appropriate lifestyle, and making one or two changes you will create a better balance within yourself, and find that you achieve much more.
Elements : ether and air.
Climate : dry and cold.
Principle : movement.
Emotions : fearful, anxious, apprehensive, sensitive, timid, lacking confidence, slightly nervous, changeable.
Systems most affected by excess vata: the nervous system and also the colon.
Symptoms of excess vata: flatulence, back pain, problems with circulation, dry skin, outbreaks of arthritis, constipation, and
nerve disorders.
The vata body type is usually thin and narrow. Vatas do not gain weight easily and are often restless by nature, especially when they are busy and active. They have dry hair and cool skin and a tendency to feel the cold. Their levels of energy are erratic, and they have to be very careful not to exhaust themselves, leading to inconsistency. They may find it quite hard to relax, which can lead to an overactive mind and insomnia.
Vata symptoms will be changeable, being cold by nature and therefore worse in cold weather Any pain will worsen during change. Vata people can suffer from wind, low back pain, arthritis and nerve disorders because of their individual restless nature, certainly require a regular intake of nourishment, and they should sit down to eat or drink at regular times. Careful exercise should always be taken in moderation, clearly maintaining a gentle, regular; well-worked out routine that will help to keep the mind focused, and in perfect harmony with the body.
Click here to find more about Vata People's Dietary Guide
http://www.byhealth.com/vata-peoples-deitary-tips
Vata People's Deitary Tips
Vata people must always be quite careful, but not to the point that cooking suddenly becomes something of a difficult problem.
The easy-to-follow, basic guidelines are as follows.
- You must avoid all kinds of fried foods, no matter how tempting and you should eat at regular intervals, Irregular, huge meals are to be avoided at all costs.
- To reduce any excess vata then follow the vata diet and recommendations in your eating and living plan.
- Always attempt to avoid any foods and other items that are not listed as far as it possible.
- If animal products are a part of your diet, they should be used strictly in moderation
Herbs and Spices

Almond essence, asafoetida (hing), basil leaves, bay leaves, cardamom pods, coriander (cilantro), fennel, fresh ginger, marjoram, mint, nutmeg, oregano, paprika, parsley, peppermint, spearmint, tarragon, thyme, turmeric and vanilla.
Grains and Seeds
Oats (cooked), pumpkin seeds, quinoa, rice (this includes all kinds and varieties), sesame seeds, sprouted wheat bread, sunflower seeds and wheat.
Nuts, Meat and fish

almonds, brazil nuts, cashews, hazelnuts,
macadamias, pecans, pine nuts, pistachios
walnuts. Beef, chicken, duck, eggs, sea, fish, shrimps and turkey.
Vegetables

Artichokes, asparagus, beetroot, carrots, courgettes (zucchini), cucumber, daikon radish, green beans, leeks, okra, olives, onions (cooked), parsnips, pumpkins, radishes, spinach (cooked), swede (rutabagas), sweet potatoes, tomatoes (cooked), and fresh watercress.
Fruits

Apricots, avocados, bananas, berries, cherries, fresh coconuts, dates, fresh figs, grapefruit, grapes, lemons, limes, mangoes, melons, oranges, peaches, pineapples, rhubarb and strawberries.
Dairy Products

Cow's milk, cottage cheese, goat's milk,
goat's, cheese and soft cheese - all are to
be taken sensibly, in moderation.
Cooking Oils

Unrefined sesame oil.
Drinks

Apricot juice, carrot juice, ginger tea, grape juice, grapefruit juice, orange juice, hot dairy drinks, lemon balm tea lemonade and peach juice
Click Here for information about Pitta People's Dietary Guide
http://www.byhealth.com/pitta-peoples-dietary-tips
Click Here for information about Kapha People's Dietary Guide
http://www.byhealth.com/kapha-peoples-dietary-tips
